Atrial septal defect (ASD) is associated with pulmonary hyperperfusion and inflammation and has been linked with increased risk of pneumonia. We investigated the risk of pneumonia in patients with ASD and the impact of ASD closure in a nationwide cohort study. All adults in Denmark (n = 1,168) diagnosed with ASD from 1977 to 2009 were identified through Danish public registries. We compared the risk of hospitalization for pneumonia, use of antibiotics, and mortality with age- and gender-matched general population controls. The median follow-up from time of diagnosis was 9.6 years (range 1 to 33). Cox regression analysis showed that both patients with closed (n = 863) and unclosed (n = 305) ASD had a higher risk of hospitalization for pneumonia (adjusted hazard ratios [HRs] 2.8, 95% confidence interval [CI] 2.3 to 3.5 and 3.1, 95% CI 2.4 to 4.0, respectively) than controls. Patients with ASD also used more antibiotics (adjusted HR for closure 1.4, 95% CI 1.3 to 1.5 and adjusted HR for no closure 1.4, 95% CI 1.2 to 1.6) than the controls. Antibiotic use normalized (adjusted HR 1.1, 95% CI 1.0 to 1.3) and the risk of pneumonia decreased (adjusted HR 1.8, 95% CI 1.1 to 3.0) within 5 years after closure. The proportion of patients with ASD with pneumonia-related death (8.4%) was comparable with that of the general population (9.5%). In conclusion, patients with ASD had a substantially higher risk of hospitalization for pneumonia and used more antibiotics than the general population. The pneumonia risk diminished, but did not completely normalize, 5 years after closure.
Atrial septal defect (ASD) is one of the most common congenital heart diseases diagnosed in adulthood. It is often accompanied by significant hemodynamic changes and right ventricular dilatation, and typical symptoms include dyspnea, fatigue, and palpitations. Pneumonia has been reported to be a frequent event in patients with ASD aged ≥60 years, but the risk of pneumonia in patients with ASD and the underlying pathogenesis is poorly characterized. An interatrial shunt gives rise to volume overload of the right heart, pulmonary hyperperfusion, and pressure elevation in the lungs. The subsequently increased vascular resistance in the lungs induces vascular remodeling and endothelial proliferative changes, which could increase the risk of pneumonia in patients with ASD. It is not known whether ASD closure significantly changes the inflammatory reaction in the lungs and if it changes the risk of respiratory infections. Pneumonia is one of the top 5 causes of death in the Western world. The mortality risk from pneumonia for patients with ASD has not been investigated, although Attie et al suggest that mortality risk from pneumonia is increased in patients who have not been treated for their ASD. In this nationwide, population-based cohort study, we compared the risk of pneumonia in the general population with the risk of pneumonia in adult patients with unclosed ASD as well as ASD closed by surgery or with a transcatheter technique. We also examined pneumonia-related mortality of adult patients with ASD.
Methods
This study was based on national medical registries in Denmark. The Danish health-care system is publically funded and, for the most part, free of charge. Data from all hospitals are gathered in nationwide public registries, which may be cross-linked using the unique personal identification number provided for every inhabitant since 1968.
Information on dates of birth, immigration, and death was identified in the Danish Civil Registration System. We used the Danish National Patient Registry (DNPR) to identify all patients born before 1993 and diagnosed with ASD ( Supplementary Appendix A ) from the beginning of the registration period in 1977 and up to 2009. The DNPR contains information on all hospital admissions in Denmark, dates of admission and discharge, surgical procedures, and discharge diagnoses coded according to the International Classification of Diseases . The eighth edition was used until 1993 after which the tenth version has been used. Only patients aged ≥18 years at the time of diagnosis were included in the study, and follow-up was continued until January 1, 2011. Patients with concomitant congenital heart disease were excluded, except those with unspecified congenital heart disease or patent ductus arteriosus, because this disease was thought to be of no relevance in adulthood ( Supplementary Appendix A ).
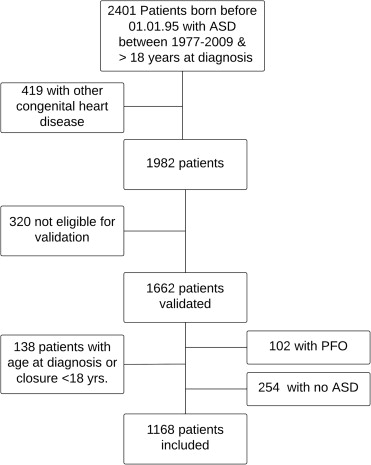
The ASD diagnoses were validated by review of the relevant medical records. Two physicians independently reviewed the records, and a pediatric cardiologist was consulted in case of discrepancy between the 2 reviewers. Only patients with a confirmed ASD diagnosis were included in this study. Patients were excluded if the defect was described as a persistent foramen ovale. Inclusion of patients is shown in Figure 1 .
For every verified patient with ASD, 10 subjects from the general population were matched on gender and birth year using the Danish Civil Registration System. We used the DNPR to identify all hospital admissions or outpatient contacts due to pneumonia since 1977 and up to January 1, 2011. Outcomes included pneumonia of all bacterial and viral types, lung abscesses, and lung empyema ( Supplementary Appendix A ). Pneumonia within 30 days after closure of the defect was ignored because of the increased risk of pneumonia directly related to the procedure.
Use of antibiotics outside hospitals defined as at least 1 redeemed prescription for antibiotics was assessed using data from the Danish National Prescription Registry ( Supplementary Appendix B ). The Danish National Prescription Registry contains information on all prescription drugs redeemed from Danish community pharmacies since 1994. It contains individual-level information on the Anatomical Therapeutic Codes on prescriptions dispensed to all subjects including residents at care facilities. We used redeemed prescriptions for antibiotics used for treatment of respiratory diseases (penicillin, β-lactam antibiotics, macrolides, aminoglycosides, quinolones, cefuroxime, and vancomycin) as an indicator of infections treated by general practitioners. This allowed us to obtain a measure of pneumonia treated outside the hospitals. Information on indication for antibiotic use is not available in the Danish National Prescription Registry.
Mortality within 2 weeks after a diagnosis of pneumonia was defined as a pneumonia-related death. Death after use of antibiotics without a diagnosis of pneumonia was considered unrelated to pneumonia because of the lack of information on the indication for use of antibiotics. Previous hospital contacts with chronic lung disease, ischemic heart disease, diabetes, pulmonary heart disease, cerebrovascular events, arrhythmia, and hypertension were identified in the DNPR and described as baseline characteristics if a diagnosis was registered before or at the time of the ASD diagnosis ( Supplementary Appendix A ). These diseases are all reported to be related to ASD and/or to be risk factors for pneumonia. Patients with Eisenmenger syndrome and pulmonary arterial hypertension were identified and included in the analyses.
For patients with ASD with closure and for their controls, the follow-up started on the date of closure (index date for comparison cohort members). For patients with ASD with no closure and for their controls, the follow-up started on the date of diagnosis. The follow-up continued until the first diagnosis with pneumonia, death, immigration, or the end of follow-up (January 1, 2011), whichever came first.
First we used Fine and Gray’s competing risk regression analysis to compute 10-year cumulative incidences of hospital admission for pneumonia with time from closure as an underlying time scale and death as a competing risk. This was also performed for patients with no closure from date of diagnosis. Second, we used Cox proportional regression analysis to compute hazard ratios (HRs) for the time to first hospital admission (in- or out-patient contacts in the hospital) for pneumonia in patients with ASD beginning at the time of diagnosis (or at 30 days after closure for those with closure), comparing them with the general population cohort using age as the underlying time scale. Analyses were stratified by age group at closure and were adjusted for gender, chronic lung disease, and hypertension. We graphically verified the assumption of proportional hazards with log-minus-log plots.
Long-term outcome was calculated for those with closure with entry at 5 years after closure and terminating at the end of follow-up. Third, incidence of pneumonia within the first 6 months after closure was compared between those undergoing catheter treatment and those with surgery. The adjusted HR for pneumonia after the first 6 months was estimated comparing the catheter-based treatment group directly with the surgery group using Cox regression analysis. Fourth, the adjusted HR of the first prescription with antibiotics was estimated at the time of diagnosis (or beginning 30 days after closure for those with closure).
Fifth, the rate of hospital contacts with pneumonia per 100 person-years was computed for the patients with ASD and population controls 5 years before and 5 years after closure (or diagnosis for those without closure). Similarly, the rate of use of antibiotics per 100 person-years was computed before and after closure or diagnosis in patients with ASD and healthy controls. All hospital contacts for pneumonia were included in the analyses; however, only hospital contacts separated by >30 days were considered to represent independent pneumonia episodes. Similarly, all filled antibiotic prescriptions were included, but only prescriptions separated by >14 days were considered to reflect independent episodes. Separate analyses of HR were done in patients with no closure after excluding patients with PAH or Eisenmenger. All analyses were performed using Stata 12 (StataCorp LP, Texas). This study was approved by the Danish Data Protection Agency (j.nr. 2010-41-4649) and the National Board of Health (j.nr. 7-604-04-2/193/KWH).
Results
The inclusion criteria were met by 1,168 patients who had been diagnosed at 1 of 80 hospitals in Denmark since 1977 ( Figure 1 ). The majority (74%) had been diagnosed in 1 of the 4 Danish university hospitals. The median follow-up time was 9.6 years (range 1 to 33.3). Patients with ASD were grouped according to whether they underwent closure or not during follow-up ( Table 1 ). Most patients were diagnosed after the age of 40 years (mean age at the time of diagnosis was 47.4).
| Variable | ASD Total | ASD Closed | ASD Not Closed | Comparison Cohort |
|---|---|---|---|---|
| (n = 1168) | (n = 863) | (n = 305) | (n = 11609) | |
| Female | 739 (63%) | 553 (64%) | 186 (61%) | 7387 (64%) |
| Mean age on 31 Dec 2012 in patients alive (years) | 63.4 ± 0.5 | 61.1 ± 0.6 | 69.4 ± 1.2 | 63.4 ± 0.2 |
| Age groups at diagnosis (years) | ||||
| <40 | 423 (36%) | 340 (39%) | 83 (27%) | 4219 (36%) |
| >40 | 745 (64%) | 523 (61%) | 222 (73%) | 7390 (64%) |
| Mean age at closure (years) | 45.4 ± 0.5 | |||
| Chronic lung disease ∗ | 50 (4%) | 29 (3%) | 21 (7%) | 253 (2%) |
| Diabetes mellitus ∗ | 34 (3%) | 18 (2%) | 16 (5%) | 214 (2%) |
| Pulmonary heart disease ∗ | 38 (3%) | 26 (3%) | 12 (4%) | 9 (0.07%) |
| Eisenmenger syndrome | 6 (0.5%) | 0 (0%) | 6 (2%) | 0 (0%) |
| Systemic hypertension ∗ | 108 (9%) | 61 (8%) | 32 (10%) | 409 (4%) |
| Coronary heart disease ∗ | 115 (10%) | 77 (10%) | 38 (12%) | 379 (3%) |
| Cerebrovascular events ∗ | 87 (7%) | 65 (8%) | 22 (7%) | 176 (2%) |
| Arrhythmia ∗ | 164 (14%) | 115 (15%) | 49 (16%) | 163 (1.5%) |
∗ Co-morbidities registered before or at the time of atrial septal defect diagnosis. Pulmonary heart disease: pulmonary arterial hypertension, pulmonary heart disease, and chronic thromboembolic heart disease.
Pneumonia admissions were observed in 240 patients with ASD (21%) and in 1,150 controls (10%). Of the patients without closure, 79 patients (26%) had at least 1 hospital admission with pneumonia. Of the patients with closure, 161 patients (19%) in total had at least 1 admission with pneumonia. After closure, 111 patients with ASD (13%) had at least 1 admission with pneumonia. Bacterial pneumonia accounted for 90% of all incident pneumonia-related hospital contacts in the entire population (88% in the ASD group).
The 10-year cumulative incidence of hospital admission for pneumonia in patients with ASD after closure was 11% (9% to 14%) compared with 4% (3% to 4.5%) in the matched comparison cohort. The 10-year cumulative incidences were greater in the patients with ASD without closure (34%; 25% to 44%) and in their matched comparison cohort (16%; 13% to 18%), but these 2 groups were on average 8 years older than the patients with closure.
Ten patients (1%) had pneumonia within the first 30 days after closure. Most had pneumonia shortly after surgery ( Figure 2 ). Patients undergoing surgery had a higher risk of hospital admission with pneumonia in the first months after closure than patients who underwent catheter-based treatment. In contrast, the risk after 6 months appeared higher for those with catheter-based treatment, although not reaching statistical significance (adjusted HR for age at closure, pulmonary heart disease, and chronic lung disease: 1.25, 95% confidence interval [CI] 0.96 to 1.62).




