His Bundle pacing (HBP) restores electrical synchronization in left bundle branch block (LBBB); however, the underlying mechanisms are poorly understood. We examined the relation between native QRS axis in LBBB, a potential indicator of the site of block, and QRS normalization in patients with LBBB. Data from patients (n = 41) undergoing HBP at 3 sites were studied (68 ± 13 years, 13 women). Study criteria included strictly defined complete LBBB and successful implantation of a permanent HBP lead. Preprocedure and postprocedure electrocardiograms were reviewed independently by 2 blinded readers. QRS axis and duration were measured to the nearest 10° and 10 ms, respectively. QRS narrowing or normalization was the primary end point. Of 29 patients meeting study criteria, 9 had frontal plane QRS axes between −60° and −80°, 10 from −40° to 0°, and 10 from +1° to +90°. QRS narrowing occurred in 24 patients (83%, 44 ± 34 ms, p <0.05). Percent QRS narrowing by axis were 26 ± 19%, 29 ± 25%, and 28 ± 23%, respectively. No correlation between prepacing QRS axis and postpacing narrowing was identified ( r 2 = 0.001, p = 0.9). In patients with or without QRS normalization after HBP, mean QRS duration was 155 ± 21 vs 171 ± 8 ms, respectively, p = 0.014. HBP induces significant QRS narrowing in most patients and normalization in patients with shorter baseline QRS duration. In conclusion, the lack of correlation between native QRS axis and narrowing suggests that proximal His-Purkinje block causes most cases of LBBB, or that additional mechanisms underlie HBP efficacy. Further studies are needed to better understand how to predict those patients in whom HBP will normalize LBBB.
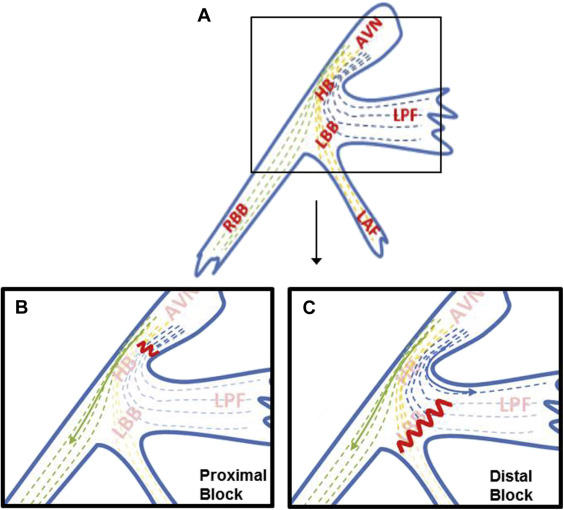
Left bundle branch block (LBBB) causes asynchronous contraction of the left ventricle (LV), which may potentially lead to eventual global LV dysfunction. Cardiac resynchronization therapy has emerged as a technique to overcome this electrical delay and has been associated with a reduction in all-cause mortality and nonfatal heart failure events. The idea of resynchronization and its clinical benefits has been extrapolated to support His bundle pacing (HBP) in patients with LBBB and cardiomyopathy. HBP has been shown to achieve significant QRS narrowing, with improved LV ejection fraction, New York Heart Association functional class, and cardiopulmonary reserve. The mechanisms underlying HBP-mediated improvement in conduction remain poorly understood and have been explained by the concept of longitudinal dissociation that fibers within the His bundle are predestined for the left and right bundle branches ( Figure 1 ). Given the well-described anatomy of the proximal His-Purkinje system, fibers exiting into the left posterior fascicle (LPF) before the site of block will result in earlier activation of the posterior-inferior LV, and hence, a left or extreme left axis deviation ( Figure 1 ). Based on the concept of longitudinal dissociation and the anatomy of the HB, we hypothesized that preprocedure extreme left axis deviation indicates distal His-Purkinje block and a lower likelihood that HBP would normalize the QRS duration.
Methods
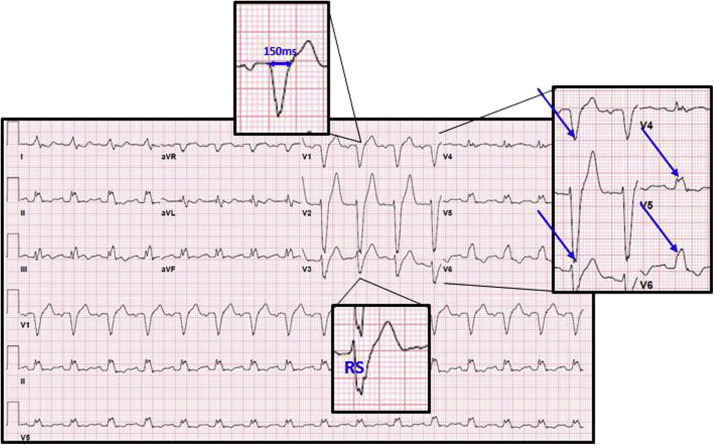
The study was approved by the institutional review board at the 3 centers. Data from 41 patients who underwent permanent HBP at these sites were evaluated retrospectively and included 17 patients from Geisinger Clinic (site 1), 14 from University of Vermont (site 2), and 10 from University of California, Los Angeles (site 3). The study period included 7 years of implantation (2008 to 2015). Patients who met a strict criteria for complete LBBB (QRS duration ≥140 ms in men or 130 ms in women; a QS or RS in leads V1 or V3; and a mid-QRS slowing or notching in ≥2 of the leads V1, V2, V5, V6, I, or aVL) had an indication for pacing or cardiac resynchronization, and who underwent a successful implantation of an HBP lead were included in this study ( Figure 2 ). Criteria for LBBB were made from a standard 12-lead electrocardiogram (ECG; 25 mm/s paper speed) or ECGs recorded using an electrophysiological mapping system (CardioLab; GE Healthcare, Ohio).
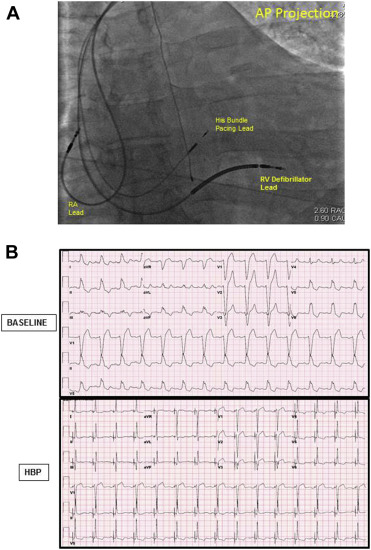
After femoral venotomy, a multipolar catheter was advanced to the region of the His bundle and used to map a discrete His potential. Using standard lead and device implantation techniques, a defibrillator lead was placed into the right ventricle for patients undergoing cardiac resynchronization therapy device implantation. Next, using a SelectSite C304 or C315 catheter system (Medtronic, Minneapolis, Minnesota), a SelectSecure 3830 lead (Medtronic) was secured to a site demonstrating a discrete His potential, guided by the multipolar catheter ( Figure 3 ). An atrial lead and generator were placed in the standard fashion. Device programming was at the discretion of the implanting physician.
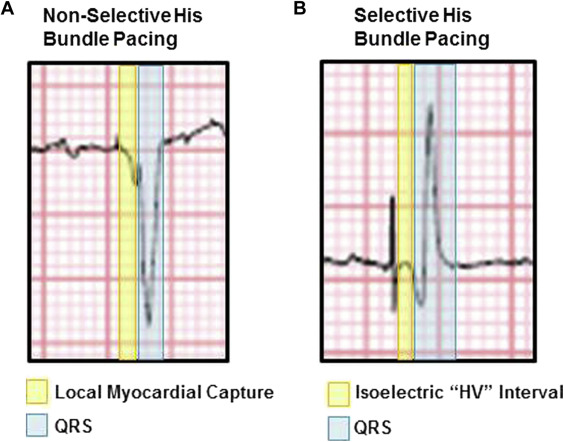
Of the patients who met study criteria, pre-HBP procedure ECGs were evaluated by 2 blinded readers in an independent ECG core laboratory. Native QRS axis was measured to the nearest 10°, and preprocedure QRS duration was measured to the nearest 10 ms. Postprocedure ECGs were deidentified. The same 2 blinded readers measured postprocedure QRS to the nearest 10 ms. Any discordant measurements between readers were reread in a group conference where a third blinded reader was present. On postprocedure ECGs and electrophysiologic tracings, QRS was measured from the onset of the first deviation from baseline for selective HBP (after the His-ventricular, or “HV”, interval) and from the onset of steepest deflection in nonselective HBP ( Figure 4 ).
The primary study outcome was the degree of QRS narrowing with HBP (absolute narrowing and percent narrowing) relative to the mean QRS axis in LBBB at baseline. The secondary outcomes were the relation between QRS narrowing and QRS axis, and the relation between QRS narrowing and ischemic versus nonischemic cardiomyopathy.
Data are expressed as mean ± SD. All indexes reported were measured from consistent tracings without artifact or loss of capture. The study data were normally distributed, and paired comparisons were made using the Student t test. Data from ≥2 groups were compared using the one-way analysis of variance. A p value ≤0.05 was considered statistically significant. Correlation between QRS narrowing and mean native QRS axis or preprocedure QRS duration was determined using linear regression. Correlation between QRS narrowing and type of cardiomyopathy was determined using one-way analysis of variance, whereas normalization was evaluated using Fisher’s exact test. Analyses were performed using Systat Software, version 13 (San Jose, California).
Results
Of the 41 patients studied, 29 patients fulfilled study criteria (including strict LBBB as defined previously) and were included in the study ( Figure 5 ). Sixteen patients were men and 13 were women. The frontal plane axis of 9 patients ranged from −60° to −80°, 10 from −40° to 0°, and 10 from +1° to +90° ( Table 1 ).
| Number | % | |
|---|---|---|
| Total pre-procedure patients included | 29 | 100% |
| Age (Years) | 68±13 | |
| Women | 13 | 41% |
| LVEF (%) | ||
| <25 | 9 | |
| 25-35 | 9 | |
| 36-45 | 3 | |
| >45 | 6 | |
| Cardiomyopathy | ||
| Nonischemic | 10 | 34% |
| Ischemic | 8 | 28% |
| Preserved ejection fraction | 4 | 14% |
| Unknown | 7 | 24% |
| Frontal Plane Axis: | ||
| Extreme left axis deviation (-0° to -80°) | 9 | 31% |
| Horizontal to left axis deviation (-40° to 0°) | 10 | 34% |
| Normal axis (+10° to +90°) | 10 | 34% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


