The heart rate at rest (HR) is a predictor of cardiovascular (CV) mortality. However, its effect on nonfatal CV events is unknown. The aim of the present post hoc analysis of the Treating New Targets (TNT) trial was to assess the effect of the HR at rest on major CV events in patients with stable coronary heart disease. A total of 9,580 subjects were included in the present analysis and were followed up for a median of 4.9 years. The rate of major CV events was 11.9% in those with a baseline HR of ≥70 beats/min versus 8.8% in those with a baseline HR of <70 beats/min. An increased HR at rest was associated with CV events, even after adjustment for differences in baseline characteristics (unadjusted hazard ratio 1.16 for every 10-beats/min increase, 95% confidence interval [CI] 1.10 to 1.23, p <0.0001; adjusted hazard ratio 1.08 per 10-beats/min increase, 95% CI 1.02 to 1.16, p = 0.018). A HR ≥70 beats/min was a significant independent predictor of all-cause mortality (hazard ratio 1.40, 95% CI 1.14 to 1.71, p = 0.001) and heart failure hospitalization (hazard ratio 2.30, 95% CI 1.80 to 2.95, p ≥0.0001). However, this association was not observed for stroke or myocardial infarction (p = 0.11 and p = 0.68, respectively). In conclusion, in patients with stable coronary heart disease, every 10-beats/min increase in the HR at rest was associated with an 8% increase in major CV events. In particular, a HR at rest of ≥70 beats/min was associated with a 40% increased risk of all-cause mortality and more than doubled the risk of heart failure hospitalization, but not the risk of stroke or myocardial infarction.
An increased heart rate (HR) at rest has been associated with worse outcomes in patients with hypertension, coronary heart disease (CHD), and left ventricular dysfunction, as well as in those without known cardiovascular (CV) disease. The possible mechanisms by which an increased HR mediates CV disease include increased sympathetic tone and changes in vascular shear stress, which might accelerate atherosclerosis. However, most previous studies have only reported fatal outcomes, and the association between increased HR and nonfatal CV events is less well understood. Moreover, it is still unclear whether the effect of an increased HR is independent of other co-morbidities. The aim of the present post hoc analysis of the Treating to New Targets (TNT) study was to determine the effect of the HR at rest on the incidence of major CV events in a group of patients with stable CHD and, in particular, to examine the differences between all-cause mortality, myocardial infarction (MI), heart failure (HF), and stroke outcomes.
Methods
The design of the TNT study has been described in detail previously. All patients gave written informed consent, and the study was approved by the research ethics committee or institutional review board at each center. Eligible patients were men and women 35 to 75 years old who had clinically evident CHD, defined by one or more of the following: previous MI, previous or current angina pectoris with evidence of atherosclerotic CHD, or a history of coronary revascularization. The exclusion criteria have been previously described in detail. Eligible patients with low-density lipoprotein cholesterol levels of 130 to 250 mg/dl without treatment underwent an 8-week run-in phase of open-label treatment with 10 mg/day of atorvastatin. At the end of the run-in phase, the participants with a low-density lipoprotein level <130 mg/dl were randomized in a double-blind fashion to 80 mg/day or 10 mg/day of atorvastatin. The baseline HR at rest was measured with the patient in the supine position using 12-lead electrocardiography. The primary end point was the occurrence of a major CV event, defined as CHD death, nonfatal MI, resuscitated cardiac arrest, or stroke. Secondary end points included all-cause mortality, nonfatal MI, fatal and nonfatal stroke, and HF hospitalization. Hospitalization for HF was defined according to the following criteria: (1) the patient was hospitalized with an admission diagnosis of HF and demonstrated signs and symptoms consistent with this clinical diagnosis; (2) the cause of HF was related to impaired left ventricular emptying or filling characteristics; and (3) the cause of HF was not temporally related to an acute MI. An independent end-points committee adjudicated all potential end points in a blinded fashion.
Of the 10,001 patients randomized in the TNT study, 9,580 had complete data available for the baseline HR and all analyzed clinical predictor variables and were thus included in the present post hoc analysis. The HR at rest was examined as a continuous variable, dichotomized into ≥70 versus <70 beats/min, and further grouped into quartiles to cover the range in HR seen in our population. The cutoff of 70 beats/min was selected prospectively according to previous studies, which have demonstrated a steep increase in the associated risk with HRs greater than this value. Differences in the baseline characteristics in the participants with a HR of ≥70 versus <70 beats/min were determined using 2-sample t tests for continuous variables and Fisher’s exact test for categorical variables.
The association between the clinical predictors and the primary outcome was initially examined using univariate Cox proportional hazards models. A multivariate Cox proportional hazards model was then constructed, adjusting for the following clinical covariates: age, gender, race, systolic and diastolic blood pressure, body mass index, current smoking, history of hypertension, diabetes, MI, angina, cerebrovascular accident, peripheral vascular disease, HF, coronary revascularization, the use of β-blocker medications, low-density lipoprotein and high density lipoprotein cholesterol, and triglyceride level. To assess the relation between HR and the secondary end points, multivariate Cox proportional hazards models were constructed, considering all clinical covariates included in the primary analysis and retaining the covariates that were significant at a level of p <0.10 on univariate analyses. Finally, the role of the randomized treatment assignment was examined, and the potential interaction between atorvastatin treatment allocation and HR was tested.
The primary and secondary end points were subsequently analyzed by baseline HR group from the point of the first dose of the study drug to the first event according to the Kaplan-Meier method, and log-rank tests were used to compare the time-to-event distributions by baseline HR groups.
The investigators had full access to, and take full responsibility for, the integrity of the data. All investigators have read and agreed to this report as written.
Results
A total of 9,580 patients with available baseline clinical characteristics were included in the present analysis and were followed up for a median of 4.9 years. At baseline, 21% had a HR at rest of ≥70 beats/min, and 79% had a HR of <70 beats/min. The clinical characteristics of the groups are listed in Table 1 .
| Variable | HR (beats/min) Group | p Value † | |
|---|---|---|---|
| <70 (n = 7,573; 3,803/3,770 ⁎ ) | ≥70 (n = 2007; 989/1,018 ⁎ ) | ||
| Heart rate (beats/min) | 57 ± 7 | 77 ± 7 | — |
| Age (years) | 61.1 ± 8.7 | 60.7 ± 9.0 | 0.071 |
| Men | 6,231 (82.3%) | 1,544 (76.9%) | <0.0001 |
| White | 7,154 (94.5%) | 1,866 (93.0%) | 0.014 |
| Systolic blood pressure (mm Hg) | 130 ± 17 | 132 ± 16 | 0.0001 |
| Diastolic blood pressure (mm Hg) | 78 ± 9 | 79 ± 9 | <0.0001 |
| Body mass index (kg/m 2 ) | 28.3 ± 4.3 | 29.4 ± 5.2 | <0.0001 |
| Current smoker | 897 (11.8%) | 359 (17.9%) | <0.0001 |
| Former smoker | 4,845 (64.0%) | 1,227 (61.1%) | 0.019 |
| Systemic hypertension | 4,030 (53.2%) | 1,151 (57.3%) | <0.0001 |
| Diabetes mellitus | 959 (12.7%) | 461 (23.0%) | <0.0001 |
| Myocardial infarction | 4,406 (58.2%) | 1,165 (58.0%) | 0.92 |
| Angina pectoris | 6,198 (81.8%) | 1,621 (80.8%) | 0.27 |
| Cerebrovascular accident | 355 (4.7%) | 133 (6.6%) | <0.0001 |
| Peripheral vascular disease | 840 (11.1%) | 276 (13.7%) | 0.0012 |
| Heart failure | 484 (6.4%) | 240 (12.0%) | <0.0001 |
| Coronary revascularization | <0.0001 | ||
| Angioplasty | 4,208 (55.6%) | 988 (49.2%) | |
| Bypass surgery | 3,365 (44.4%) | 1,078 (53.7%) | |
| Medications | |||
| β Blocker | 4,478 (59.1%) | 691 (34.4%) | <0.0001 |
| Angiotensin-converting enzyme inhibitor | 1,947 (25.7%) | 659 (32.8%) | <0.0001 |
| Calcium channel blocker | 2,002 (26.4%) | 575 (28.7%) | 0.05 |
| Digitalis | 56 (0.7%) | 26 (1.3%) | 0.02 |
| Cholesterol (mg/dl) ‡ | |||
| Total | 173.4 ± 23.4 | 178.9 ± 24.3 | <0.0001 |
| Low-density lipoprotein | 96.8 ± 17.3 | 99.8 ± 18.0 | <0.0001 |
| Triglycerides | 147.3 ± 68.9 | 160.6 ± 74.5 | <0.0001 |
| High-density lipoprotein | 47.3 ± 10.8 | 47.3 ± 11.3 | 0.84 |
⁎ Number of patients assigned to atorvastatin 80 mg/atorvastatin 10 mg.
† p Values determined using 2-sample t test for continuous variables and Fisher’s exact test for categorical variables.
‡ Baseline lipid values were measured at the end of the atorvastatin 10-mg/day run-in period.
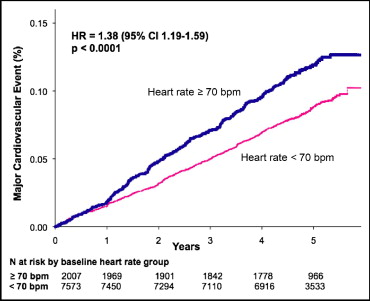
Of the 7,573 patients with a baseline HR of <70 beats/min, 665 (8.8%) experienced a major CV event during follow-up. Of the 2,007 patients with a baseline HR of ≥70 beats/min, 239 (11.9%) experienced a major CV event (hazard ratio 1.38, 95% confidence interval [CI] 1.19 to 1.59, p <0.0001). In the time-to-event analyses, a HR ≥70 beats/min was associated with significantly greater incidence rates of major CV events compared to a HR of <70 beats/min (log-rank test, p <0.0001; Figure 1 ). After adjustment for differences in the baseline characteristics, a HR at rest of ≥70 beats/min remained a borderline significant predictor of major CV events (hazard ratio 1.16, 95% CI 0.99 to 1.36, p = 0.06). On univariate analyses, the HR as a continuous variable was a significant predictor of major adverse CV events (hazard ratio 1.16 for every 10-beats/min increase, 95% CI 1.10 to 1.23, p <0.0001). After adjustment for the differences in baseline characteristics, the HR at rest remained a significant independent predictor of major CV events (hazard ratio 1.08 for every 10-beats/min increase, 95% CI 1.02 to 1.16, p = 0.01; Table 2 ). Potential confounders included in the multivariate model have been listed in the “Methods” section.
| Clinical Characteristics | Univariate Model | Multivariate Model | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| Heart rate (per 10 beats/min) | 1.16 (1.10–1.23) | <0.0001 | 1.08 (1.02–1.16) | 0.01 |
| Age (years) | 1.02 (1.01–1.02) | <0.0001 | 1.02 (1.01–1.03) | 0.0002 |
| Men | 1.20 (1.01–1.44) | 0.039 | 1.40 (1.16–1.70) | 0.0006 |
| White | 0.82 (0.64–1.07) | 0.14 | 0.91 (0.69–1.18) | 0.47 |
| Systolic blood pressure (mm Hg) | 1.01 (1.01–1.01) | <0.0001 | 1.01 (1.00–1.01) | 0.02 |
| Diastolic blood pressure (mm Hg) | 1.00 (1.00–1.01) | 0.48 | 1.00 (0.99–1.01) | 0.72 |
| Body mass index (kg/m 2 ) | 1.03 (1.02–1.05) | <0.0001 | 1.02 (1.00–1.03) | 0.04 |
| Current smoker | 1.60 (1.36–1.89) | <0.0001 | 1.66 (1.39–1.99) | <0.0001 |
| Former smoker | 0.89 (0.78–1.02) | 0.09 | ||
| Systemic hypertension | 1.58 (1.38–1.81) | <0.0001 | 1.28 (1.10–1.48) | 0.0001 |
| Diabetes mellitus | 1.823 (1.57–2.13) | <0.0001 | 1.40 (1.18–1.65) | <0.0001 |
| Myocardial infarction | 1.58 (1.38–1.82) | <0.0001 | 1.60 (1.39–1.85) | <0.0001 |
| Angina pectoris | 1.36 (1.13–1.64) | 0.001 | 1.37 (1.13–1.66) | 0.001 |
| Cerebrovascular accident | 2.45 (1.99–3.01) | <0.0001 | 1.75 (1.41–2.18) | <0.0001 |
| Peripheral vascular disease | 1.88 (1.59–2.22) | <0.0001 | 1.29 (1.08–1.54) | 0.006 |
| Heart failure | 2.27 (1.89–2.72) | <0.0001 | 1.51 (1.24–1.83) | <0.0001 |
| Coronary revascularization | ||||
| Angioplasty | 0.95 (0.84–1.09) | 0.47 | 1.04 (0.90–1.20) | 0.60 |
| Bypass surgery | 1.40 (1.23–1.60) | <0.0001 | 1.22 (1.05–1.42) | 0.01 |
| Use of β blocker | 1.06 (0.93–1.21) | 0.37 | 1.08 (0.93–1.24) | 0.31 |
| Cholesterol (mg/dl) | ||||
| Total | 1.00 (1.00–1.01) | 0.03 | ||
| Low-density lipoprotein | 1.01 (1.00, 1.01) | 0.0003 | 1.01 (1.00, 1.01) | 0.002 |
| Triglycerides | 1.00 (1.00–1.00) | <0.0001 | 1.00 (1.00–1.00) | 0.46 |
| High-density lipoprotein | 0.98 (0.98–0.99) | <0.0001 | 0.99 (0.98–1.00) | 0.009 |
| Atorvastatin (80 vs 10 mg) | 0.78 (0.69–0.89) | 0.0002 | 0.78 (0.68–0.89) | 0.0002 |
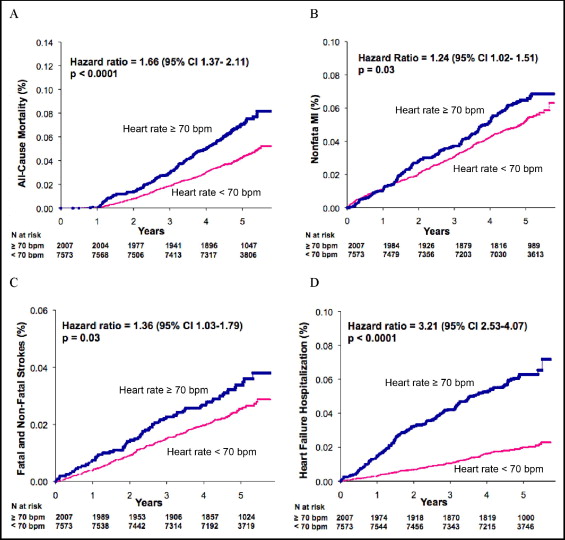
The cumulative incidence of each of the secondary outcomes, including all-cause mortality, HF hospitalization, nonfatal MI, and fatal and nonfatal stroke, is summarized in Figure 2 . A HR at rest of ≥70 beats/min was associated with increased all-cause mortality compared to a HR of <70 beats/min in the unadjusted analyses (hazard ratio 1.66, 95% CI 1.37 to 2.11, p <0.0001). After adjustment for differences in the baseline characteristics, an increased HR remained independently associated with all-cause mortality (hazard ratio 1.40, 95% CI 1.14 to 1.71, p = 0.001). Similarly, a HR at rest of ≥70 beats/min was associated with a >3-fold increased hazard of HF hospitalization (hazard ratio 3.21, 95% CI 2.53 to 4.07, p <0.0001). An increased HR remained an independent predictor of HF hospitalization, even after adjustment for potential clinical confounders, including a history of HF at baseline, more than doubling the risk of an event (hazard ratio 2.30, 95% CI 1.80 to 2.95, p <0.0001).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


