Adoption of appropriate use criteria has not had a major impact on the frequency of “rarely appropriate” tests, with the rarely appropriate tests rate remaining at ∼20% in most institutions. We sought whether access to hand-held ultrasound (HHU) could be an alternative means of reducing rarely appropriate requests. We compared 2 approaches to rarely appropriate requests; “standard transthoracic echocardiography” (SE) as requested (control) and HHU as a gatekeeper (HHU). Patients were followed up for 6 months and assessed for end points including time until scan, repeat echocardiography/cost of either strategy, new major pathology, and change in management. The most common rarely appropriate requests in both groups were assessment of infective endocarditis without positive blood cultures and precordial murmur evaluation in absence of any other signs or symptoms of cardiovascular disease. The groups had comparable age, gender, requesting physician, and inpatient versus outpatient distribution. HHU led to a 59% reduction in rarely appropriate requests requiring SE. HHU significantly reduced time to decision for inpatients (0 [interquartile range 0, 1] vs 2 days [interquartile range 1, 4], p <0.001) and total cost of echocardiography (109 ± 86 vs 181 ± 37 USD, p <0.001). New major pathology was identified in 29% and 23% of HHU and SE, respectively. There was no difference with respect to change in management. In conclusion, HHU can be an effective gatekeeper to SE for rarely appropriate echocardiograms, reducing time to echocardiography and cost while satisfying the referring physician and avoiding repeat requests for SE. HHU provides a safety net that identifies potential important findings in rarely appropriate requests.
The overutilization of echocardiography has been a significant contributor to the fourfold growth of Medicare reimbursements to cardiologists from 2000 to 2006. The appropriate use criteria (AUC) and other educational initiatives have been components of efforts to curb inappropriate use. Despite a decrease in reimbursements by 33% for echocardiography from 2006 to 2010, there is limited evidence to suggest there is a decrease in the rate of inappropriate echocardiography. Indeed, interventions targeting education and the use of point of order applications have been applied with varying degrees of success. A problem with the AUC process is that restriction of tests may be contrary to the guidelines and risks missing important pathology. New, important transthoracic echocardiography (TTE) abnormalities have been demonstrated in 17% of inappropriate studies ; 22% of rarely appropriate tests resulted in an active change in management. In the context of these observations, it is difficult to enforce an overarching prohibition on rarely appropriate requests. Although previously unconnected, hand-held ultrasound (HHU) has developed over a similar timeline to the AUC. Validation studies against standard transthoracic echocardiography (SE) show high levels of agreement for morphology, functional, and valvular assessment. Comparisons of HHU to physical examination have demonstrated superiority of the former and its cost-effectiveness. We hypothesized that HHU could be applied as a gatekeeper to SE for rarely appropriate examinations and that such a strategy would reduce numbers of SE performed and cost, identify important pathology that would have been missed if the rarely appropriate tests were cancelled, and facilitate decision making and patient management.
Methods
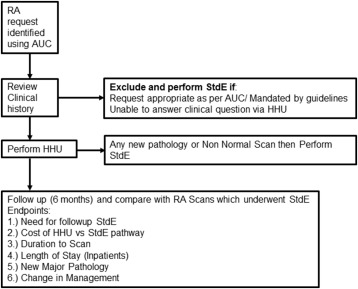
This was a case-control study designed to compare an HHU-based approach to rarely appropriate tests to the current SE-based system. It was performed across 2 hospitals and included both inpatients and outpatients. Rarely appropriate requests were identified using the AUC. If the clinical history was inadequate to ascertain appropriateness, medical records were consulted. The process of canceling rarely appropriate requests is not systematic and is dependent on inpatient and outpatient waiting lists. We performed HHU on requests that were destined to be cancelled.
The study was performed from March 2015 to December 2015. All rarely appropriate requests during this time period were assessed for eligibility. Requests were excluded from analysis if deemed appropriate after review of medical records or if tests were mandated by guidelines. Requests beyond the scope of HHU were also excluded. The resulting cohort of HHU cases was case matched 2:1 to a cohort of rarely appropriate requests that had undergone SE from 2013 to 2015.
Eligible patients with rarely appropriate requests received a cardiology consultation and HHU examination performed by a cardiologist ( Figure 1 ). If the consult suggested the request was appropriate, then an SE was performed and these patients were excluded. The study was approved by the Tasmanian Human Research Ethics committee.
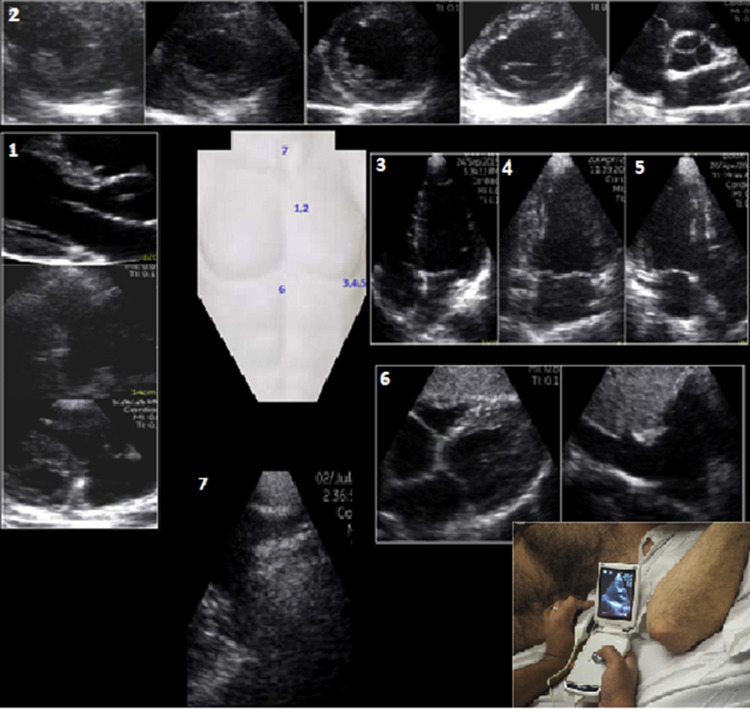
HHU was performed using the GE Vscan V1.2 hand-held device (GE Health Care, Milwaukee, Wisconsin). The HHU study protocol involved 2-dimensional grayscale and color Doppler images across all standard echocardiographic views ( Figure 2 ). Linear or area measurements were made as appropriate. Spectral Doppler data were not obtained as this feature is not available on the HHU. Severity of disease was approximated using 2-dimensional signs of severity (e.g., leaflet excursion, chamber dilatation) and size and duration of the color jet/proximal convergence zone. All HHU examinations were limited to <10-min duration. Results of the HHU study were communicated to the treating team, documented in clinical notes, or provided as a short report for outpatients.
Eligible patients went on to have a formal SE if the HHU suggested a full study was warranted, if HHU was nondiagnostic, if there was any HHU abnormality in a patient without a previous echocardiogram, or any new changes in patients with a previous examination.
The HHU cohort was case matched to a cohort of patients with rarely appropriate tests who underwent an SE. The SE examination was performed on 3 machines: GE Vivid 9 (GE Health Care, Milwaukee, Wisconsin), Phillips IE33 (Philips Medical Systems, Andover, Massachusetts), and Acuson SC2000 (Siemens, Erlangen, Germany). All SE were performed over 45 to 60 minutes by an experienced sonographer and interpreted by a cardiologist.
Patients in both HHU and SE arms were followed up for 6 months and evaluated for the end points of repeat TTE, cost of care, time to scan, length of stay (inpatients), new major TTE abnormality/incidental findings, and change in management. The cost of additional scans was incorporated into each arm. The cost of SE was 230 USD, in accordance with standard reimbursement. The cost of the hand-held device is 6,000 USD, assuming a depreciation of 750 USD per year and its use in 100 rarely appropriate requests per year, the cost per scan of the device would be 7.50 USD per rarely appropriate scan. We added to this the cost of storage of images, 15-minute time for cardiologist to perform consultation, echocardiography, and generate report to arrive at an estimate cost of 38 USD per scan. This approach is consistent with previous attempts to itemize a cost for HHU accounting for geographical variations ( Table 1 ).



