The evaluation of patients presenting to the hospital with a recent episode of chest pain suggestive of myocardial ischemia, nondiagnostic electrocardiographic findings, and normal 12-hour cardiac troponin levels remains a challenge for the clinician. We selected 1,081 consecutive patients who presented to the emergency department during 2008 for a chest pain complaint of suspected cardiac origin without significant electrocardiographic abnormalities or troponin elevation. These patients underwent either contrast-enhanced stress-echocardiography with myocardial perfusion imaging or exercise-electrocardiography within 5 days of the index admission. We analyzed their 1-year cardiac outcome (i.e., unstable angina, myocardial infarction, or cardiac death). A post test likelihood of cardiac events was determined on the basis of the results of the provocative testing. Significantly better event-free survival (log-rank p <0.0001) was found for both hard (cardiac death and nonfatal myocardial infarction) and combined (acute coronary syndrome) end points in patients with normal contrast-enhanced stress-echocardiographic findings. However, this was not the case for patients in the exercise-electrocardiographic group, for whom event-free survival was not significantly different among the 3 possible result categories (normal, indeterminate, and abnormal test findings; log-rank p = NS). In conclusion, inducible ischemia detected by contrast-enhanced stress-echocardiography predicted the 1-year incidence of acute coronary syndrome (11.3% for positive vs 0.8% for negative results). However, this was not the case for exercise-electrocardiography, with a 2.7%, 2.3%, and 2.9% 1-year incidence of acute coronary syndromes for positive, negative, and indeterminate results, respectively.
The prognostic assessment of patients presenting to the hospital with a recent episode of chest pain suggestive of myocardial ischemia but no sign of acute coronary syndrome (ACS) remains a challenge for the clinician. We analyzed and followed up all consecutive patients who had presented to the emergency medicine department during 2008 for a chest pain episode of suspected cardiac origin, without significant electrocardiographic (ECG) abnormalities or 12-hour troponin elevation and had undergone either contrast-enhanced stress-echocardiography (contrast-SE) or exercise-electrocardiography within 5 days of the index admission. The procedures and cardiac events at 1 year of mean follow-up were recorded, and the diagnostic and risk-stratifying capability of both tests were determined.
Methods
The present study was an observational outcome analysis. It was conducted at a 1,300-bed tertiary referral center. We included patients who had presented to the emergency department during 2008 for chest pain of suspected cardiac origin, normal/nondiagnostic serial ECG findings, and negative 12-hour troponin I results and had undergone either exercise electrocardiography or contrast-SE within 5 days of the index chest pain episode (during their chest pain unit stay or within the first few days after discharge). The patients who had undergone both provocative tests within 5 days of the chest pain episode were excluded. However, if the first test was performed within 5 days, but the second test was after 5 days, the patient was not excluded. In such cases, the first test only was considered for the present study. Because of the retrospective nature of the study, the choice of the provocative test was always made by the cardiologist in charge at the patient’s admission to the chest pain unit and according to the hospital guidelines. Our local chest pain unit protocol has recommended exercise electrocardiography as the first-choice provocative test when patients appear able to exercise and in the absence of known contraindications to the test. All other patients have been recommended to undergo a pharmacologic stress test. Contrast-SE was preferred over nuclear medicine tests because of local expertise, logistical reasons, and the absence of ionizing radiation. Patients initially considered for contrast-SE did not undergo the test if they presented with ≥1 of the following exclusion criteria: (1) severely reduced left ventricular ejection fraction <30%, (2) severe valvular disease, (3) sustained ventricular arrhythmias or hemodynamic instability, (4) chest pain within the previous 24 hours, (5) an inability to stop β blockers in the previous 24 hours, (6) a known allergy to sulfonamides, and (7) pregnancy or lactation. In the case of the fourth or fifth criterion, the test was postponed to the day after. The study complied with the Declaration of Helsinki and the institutional ethics committee approved the present study. All patients gave written informed consent.
The acute treatment of the patients was performed according to standard hospital protocols. All patients were assessed clinically, including history, evaluation of the cardiac risk factor profile, medication use, height and weight, and Thrombolysis In Myocardial Infarction (TIMI) risk score. The evaluation included serial 12-lead electrocardiograms and serum cardiac troponin measurements. The electrocardiograms were recorded on presentation, every 6 hours, and during any new episode of chest pain. The cardiac troponin I measurements were taken at admission and every 6 hours for up to a minimum of 12 hours after the onset of pain. The TIMI risk score was used as a guide to the pretest probability of cardiac events. A TIMI score of 0 to 1 was considered low risk; 2 to 4 intermediate risk, and ≥5 high risk. A post test likelihood of cardiac events was determined on the basis of the results of the provocative testing. A positive or negative provocative test result reclassified the patient to a high or low post test risk, respectively. An indeterminate test result classified the patient to an intermediate risk. Any additional investigations or procedures were made at the discretion of the attending physician. They included additional noninvasive imaging, as appropriate, or coronary angiography. Coronary angiography was indicated by the attending physician, who was aware of the stress test findings and was determined by clinical judgment and the presence of inducible ischemia.
Exercise electrocardiography was performed using a symptom-limited Bruce protocol performed using a treadmill with continuous monitoring of a 12-lead electrocardiogram and regular blood pressure measurements. The standard end points were used: fatigue, severe ischemia (severe angina, ≥2-mm ST-segment depression), hypertension (systolic blood pressure ≥220 mm Hg), hypotension, presyncope, or arrhythmia. Details regarding anginal symptoms, ST-segment deviation, and exercise capacity were recorded. The patients able to perform to a workload of ≥7 METs without hemodynamic compromise or ECG changes were considered to have negative test results. The patients who developed significant hypotension, arrhythmia, or ≥1 mm planar or downsloping ST-segment depression were considered to have positive test results. All other patients were considered to have indeterminate test findings.
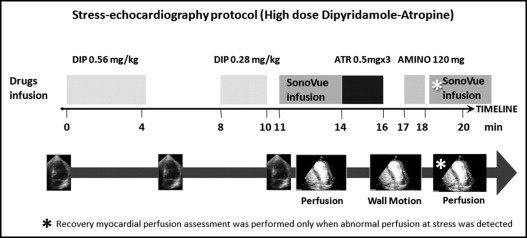
The contrast-SE protocol has been summarized in Figure 1 . The patients underwent dipyridamole-atropine echocardiography with adjunctive myocardial perfusion assessment between the end of the dipyridamole infusion (0.84 mg/kg/10 min) and the beginning of the atropine infusion. Consolidated end points and contraindications were used. The patients underwent both wall motion and myocardial perfusion studies using an iE33 echocardiograph with a S5 scan head (Philips Ultrasound, Bothell, Washington). Myocardial perfusion was assessed using SonoVue (Bracco Imaging Italia, s.r.l., Milan, Italy) as a continuous infusion (0.8 ml/min) with flash-replenishment low-mechanical index imaging. An additional SonoVue infusion (1.0 ml/min) for myocardial perfusion was performed after reversal with aminophylline only for those patients in whom a perfusion defect was detected at stress to assess the reversibility of the defect. Regional wall motion analysis was evaluated at baseline and at peak stress using a semiquantitative wall motion score (i.e., normal, hypokinesia, and akinesia) on a 17-segment model of the left ventricle. Reversible wall motion abnormality was defined as either a new dyssynergy in a region with normal function at rest or worsening of hypokinesia at rest in ≥1 segment. Normal perfusion after dipyridamole was considered present if the myocardium was fully replenished 1.5 to 2 seconds after the end of the flash impulse. The perfusion was defined as abnormal if the myocardium was not replenished after this time. The cutoff for normal replenishment after the aminophylline infusion (recovery stage) was considered 4 seconds after the flash impulse. A perfusion defect was scored as fixed or reversible according to its persistence at the recovery stage. The contrast-enhanced stress echocardiographic finding was defined as “abnormal” in the presence of ≥1 of the following in ≥1 myocardial segment: (1) reversible wall motion abnormality, (2) reversible myocardial perfusion defect, and (3) a fixed myocardial perfusion defect in patients without a previous myocardial infarction (MI). The presence of a fixed perfusion defect in the site of a known previous MI was considered a “normal” contrast-enhanced stress-echocardiographic result. All tests were evaluated off-line by 2 experienced echocardiographers.
Elective coronary angiography performed within 60 days after the tests was considered for diagnostic assessment of coronary artery disease. Any visually evident stenosis was measured using a hand-held electronic caliper (Tesa SA, Renes, Switzerland) operated with custom-developed software. The measurements are expressed as the percentage of diameter narrowing using the diameter of the nearest normal-appearing region as the reference. Coronary artery disease was defined as >50% luminal diameter stenosis in ≥1 major coronary arteries. Data were collected regarding cardiac events and additional investigations performed. A hard cardiac end point was defined as cardiac death or nonfatal MI, and an ACS combined end point was defined as unstable angina requiring unplanned revascularization, nonfatal MI, or cardiac death. Cardiac death was defined as death associated with known/suspected MI, life-threatening arrhythmia, or heart failure. Nonfatal MI was defined using the criteria of typical chest pain and elevated cardiac enzyme levels, with or without typical changes on the electrocardiogram. The follow-up data were obtained from the review of the patient’s hospital chart, electronic records, and telephone interview with the patient.
Continuous variables are expressed as the mean and standard deviation. The categorical variables are expressed as proportions. A comparison of the continuous data was done using Student’s t test. For categorical variables, a chi-square analysis was used. Kaplan-Meier curves were used to estimate the distribution of the interval to the end point. The differences between the time-to-event curves were compared to the log-rank test. A Cox proportional hazards model was used to evaluate any potentially significant predictor of cardiac events. Age, left ventricular ejection fraction, and TIMI risk score were analyzed as qualitative variables because of their varying clinical significance at different cutoff values. A value of p <0.05 was considered significant.
Results
A total of 1,081 patients satisfied the inclusion and exclusion criteria during the study period. The patients who underwent exercise-electrocardiography were younger and had a lower TIMI risk score than the patients in the contrast-enhanced stress echocardiographic group ( Table 1 ). Accordingly, cardiovascular risk factors and medication use were more prevalent in the contrast-enhanced stress echocardiographic group. Of the 536 patients in the exercise electrocardiographic group, 129 (24%) were not able to reach the 7 METs workload, without the criteria of positivity. They were classified as having indeterminate results and considered at intermediate risk of cardiac events. The patients undergoing contrast-SE had no indeterminate results. All patients with an abnormal wall motion response (n = 101) also had abnormal myocardial perfusion findings, and 94 had isolated myocardial perfusion abnormalities. Thus, the wall motion response during stress testing did not modify the final diagnostic results, which were entirely driven by the myocardial perfusion results.
| Variable | Ex-ECG (n = 536) | Contrast-SE (n = 545) | p Value |
|---|---|---|---|
| Mean age (years) | 62 ± 12 | 67 ± 11 | <0.0001 |
| Age ≥65 years | 234 (44%) | 350 (64%) | <0.0001 |
| Men | 334 (62%) | 317 (58%) | NS |
| Thrombolysis in myocardial infarction risk score | <0.0001 | ||
| 0–1 | 426 (79%) | 240 (44%) | |
| 2–4 | 110 (21%) | 305 (56%) | |
| Hereditary | 182 (34%) | 125 (22%) | <0.0001 |
| Hypercholesterolemia ⁎ | 39 (7%) | 318 (58%) | <0.0001 |
| Hypertension † | 268 (50%) | 417 (77%) | <0.0001 |
| Diabetes mellitus | 48 (9%) | 128 (24%) | <0.0001 |
| Cigarette smoking | 98 (18%) | 136 (25%) | <0.01 |
| Obesity ‡ | 43 (8%) | 75 (14%) | <0.01 |
| Myocardial infarction/known coronary artery disease or revascularization | 80 (15%) | 218 (40%) | <0.0001 |
| Medications | |||
| Aspirin | 117 (22%) | 332 (61%) | <0.0001 |
| β Blockers | 53 (10%) | 307 (55%) | <0.0001 |
| Statins | 41 (8%) | 296 (54%) | <0.0001 |
| Test results | |||
| Positive provocative test | 69 (13%) | 195 (36%) | <0.0001 |
| Indeterminate provocative test | 129 (24%) | — | |
| Negative provocative test | 338 (63%) | 350 (64%) | NS |
| Angina during the test | 90 (17%) | 57 (10%) | <0.01 |
| Cardiac events | |||
| All | 14 (2.6%) | 25 (4.6%) | NS |
| Cardiac death | 1 | 0 | NS |
| Myocardial infarction | 6 | 12 | NS |
| Unstable angina requiring percutaneous coronary intervention/coronary artery bypass grafting | 7 | 13 | NS |
⁎ Total cholesterol >180 mg/dl or treatment of hypercholesterolemia.
† Blood pressure ≥140/90 mm Hg or treatment of hypertension.
In the contrast-enhanced stress-echocardiographic group, 170 underwent coronary angiography at the discretion of the attending physician. Significant coronary artery disease was detected in 130 patients (76%). In the exercise-electrocardiographic group, 53 underwent coronary angiography at the discretion of the attending physician. Significant coronary artery disease was detected in 36 patients (68%). Table 2 lists the diagnostic data for both tests in patients who underwent coronary angiography within 2 months of the provocative test. Follow-up was completed in July 2009, with a mean follow-up period of 358 ± 127 days.
| Variable | Positive | Negative | Indeterminate (<7 METs) |
|---|---|---|---|
| Exercise-electrocardiography (n = 53) | |||
| Coronary artery disease ⁎ | 15 (TP) | 18 (FN) | 3 |
| No coronary artery disease † | 6 (FP) | 8 (TN) | 3 |
| Accuracy for coronary artery disease | >50% | 48% | |
| Contrast-SE (n = 170) | |||
| Coronary artery disease ⁎ | 125 (TP) | 5 (FN) | 0 |
| No coronary artery disease † | 18 (FP) | 22 (TN) | 0 |
| Accuracy for coronary artery disease | >50% | 86% |
In the exercise-electrocardiographic group, the median follow-up for patients who did not experience an event was 358 days. A total of 14 patients (2.6%) had experienced cardiac events during the follow-up. Hard cardiac events occurred at a median of 234 days (range 9 to 505) after the stress test and included nonfatal MI in 6 (1.1%) and cardiac death in 1 (0.2%) and were unrelated to revascularization. Unstable angina requiring unplanned revascularization was recorded in 7 patients at a median of 156 days (range 8 to 462). A total of 20 patients underwent test-driven, elective percutaneous intervention (n = 14) or coronary artery bypass (n = 6) within 2 months of exercise-electrocardiography.
In the contrast-enhanced stress-echocardiographic group, the median follow-up for patients who did not experience an event was 361 days. A total of 25 patients (4.6%) experienced cardiac events during follow-up. Hard cardiac events occurred at a median of 163 days (range 23 to 370) after the index stress test and included nonfatal MI in 12 patients (2.2%) that were unrelated to revascularization. Unstable angina requiring unplanned revascularization occurred in 13 patients at a median of 129 days (range 37 to 362). No cardiac deaths occurred; 1 patient died from a noncardiac cause. A total of 82 patients had undergone test-driven, elective, percutaneous intervention (n = 65) or coronary artery bypass grafting (n = 17) within 2 months of contrast-SE.
A statistically significant difference in the event-free survival (log-rank p <0.0001) was found for both hard (cardiac death and nonfatal MI; Figure 2 ) and combined ACS end points ( Figure 3 ) between patients with normal and abnormal findings from contrast-SE. In contrast, in patients in the exercise-electrocardiographic group, the event-free survival was not significantly different among the 3 possible result categories (normal, indeterminate, and abnormal; log-rank p = NS).




