Current task force criteria (TFC) of cardiac magnetic resonance (CMR) for the diagnosis of arrhythmogenic right ventricular cardiomyopathy (ARVC/D) were generated by comparing probands (mean age of 44 years) to healthy participants of the multi-ethnic study of atherosclerosis (mean age of 60 years). These age differences may be a selection bias because right ventricular end-diastolic volume index decreases 4.6% per decade. Moreover, fat infiltration and late gadolinium enhancement were not included. We evaluated the diagnostic accuracy of TFC using the same methodology used by the task force but comparing probands and age- and gender-matched healthy controls and considering also other morphofunctional and tissue abnormalities detected by CMR. Forty-seven probands with previous diagnosis of ARVC/D (excluding probands if CMR was used for diagnosis) were compared with 216 age- and gender-matched healthy controls. TFC had optimal specificity (100%) but poor sensitivity (20% for major and 13% for minor criteria). The presence of any pre- and post-contrast signal abnormalities had 100% specificity and 81% sensitivity. The best diagnostic accuracy (98%) was achieved by the combined evaluation of any right ventricular wall motion abnormality (excluding hypokinesia) with any signal abnormality (including left ventricular fat infiltration and late gadolinium enhancement) yielding a 100% specificity and 96% sensitivity. Left ventricular was involved in 45% of the probands. Current TFC for CMR presented optimal specificity but poor sensitivity to identify patient with ARVC/D. Signal and wall motion parameters of CMR should be considered together to achieve the best diagnostic accuracy for the diagnosis of ARVC/D.
In 2010 International Task Force criteria for the clinical diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D), the task force criteria (TFC) were modified including quantitative parameters for cardiac magnetic resonance (CMR). However, some unique capabilities of CMR, such as the detection of myocardial fat infiltration and fibrosis, that have been otherwise demonstrated to predict adverse events even in patients with suspect of ARVC/D, were not included. Current CMR criteria were generated by comparing 462 healthy controls of the multi-ethnic study of atherosclerosis (MESA) with 44 ARVC probands with a significantly different mean age (controls 60.4 ± 10 years, probands 40.4 ± 12 years). This age difference may be relevant because of the physiological decrease of right ventricular (RV) end-diastolic volume index (EDVi) between healthy controls of 40 and 60 years old. Participants in the MESA study (range age from 45 to 84 years) showed an RV EDVi decrease of 4.6% per decade. Finally, the MESA study used a fast gradient echo technique for the quantification of ventricular volumes, whereas steady-state free precession (SSFP) images provide superior contrast between blood and endocardium at the endocardial border with less blood flow dependence. The aim of this study was to (1) evaluate the diagnostic accuracy of the TFC for CMR, using the same methods of the 2010 Task Force, by comparing probands and age- and gender-matched healthy controls and using SSFP cine sequence, and (2) compare current TFC for CMR with morphofunctional and tissue abnormalities detected by CMR for the diagnosis of ARVC/D.
Methods
Forty-seven probands with previous diagnosis of ARVC/D were enrolled. To eliminate selection bias, we excluded probands if CMR was used for the diagnosis of the individual patient. A control group of 216 healthy subjects was included in the study with the following inclusion criteria: (1) absence of contraindications to CMR; (2) no personal history of cardiac and noncardiac disease; (3) no family history of genetic disease; (4) normal physical examination; (5) normal electrocardiogram; (6) normal echocardiography; (7) absence of coronary risk factors including diabetes, hypertension (defined as diastolic blood pressure 90 mm Hg, systolic blood pressure 140 mm Hg, or receiving treatment for hypertension), hyperlipidemia (abnormal lipid levels or receiving lipid-lowering therapy), obesity (defined as body mass index ≥30); and (8) subjects with referred smoke habit or drug assumption were excluded. All subjects were informed about the study protocol and provided written consent.
CMR examinations were performed using a 1.5 T Signa Cvi scanner (GE, Milwaukee, Wisconsin) with a Cardiac Phased Array 8-channel coil. For the assessment of left ventricular (LV) and RV regional wall motion (WM), ventricular volumes and mass and cine images were used with an SSFP (fast imaging employing steady-state acquisition) pulse sequence in short-axis views (from atrioventricular valve plane to the apex, 8-mm slice thickness, no gap) and in axial views (from diaphragm to the entire outflow tract, 5 mm slice thickness, no gap). The following acquisition parameters were applied: 30 phases, 10 to 25 views per segment depending on heart rate, NEX 1, field of view (FOV) 40 cm, a matrix of 224 × 224, a 45° flip angle, TR/TE ≈ 2, and a bandwidth of 125 KHz.
Double IR fast spin echo (FSE) images were acquired in the same short-axis views (8 mm slice thickness, no gap) and axial views (5 mm slice thickness, no gap) with the following parameters: NEX 1, FOV 40 cm, matrix of 256 × 256, a 90° flip angle, and a bandwidth of 62.5 KHz. The FSE images were also re-acquired using a fat saturation pulse to selectively null signals from fat.
Late gadolinium enhancement (LGE) images were acquired 10 minutes after administration of Gd-DTPA (Magnevist; Schering-AG, Germany) with a dosage of 0.2 mmol/kg in the same short-axis and para-axial views. An inversion recovery T1-weighted GRE was used with the following parameters: FOV 40 mm, slice thickness 8 mm, no gap between each slice, repetition time 4.6 milliseconds, echo time 1.3, flip angle 20°, matrix 224 × 224, reconstruction matrix 256 × 256, and one excitation. The appropriate inversion time was set to null the normal myocardium (range 250–300 milliseconds, obtained using a TI-scout).
The CMR images were independently analyzed by 3 investigators (third-level ESC accreditation for CMR, working in a CMR laboratory performing >2,500 cardiac examination per year, with >100 ARVC/D suspicion per year) who were unaware of the diagnoses.
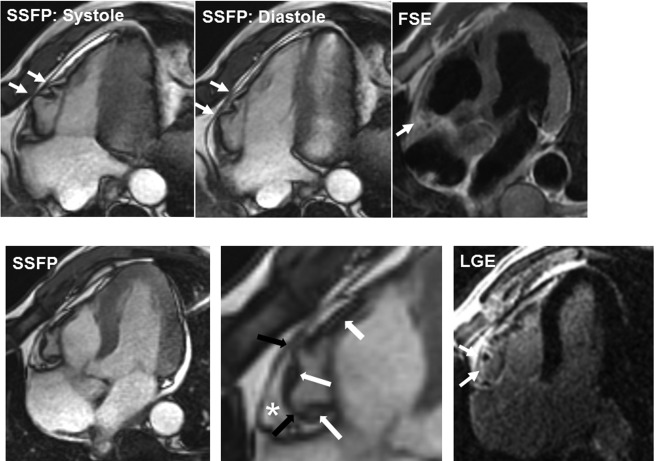
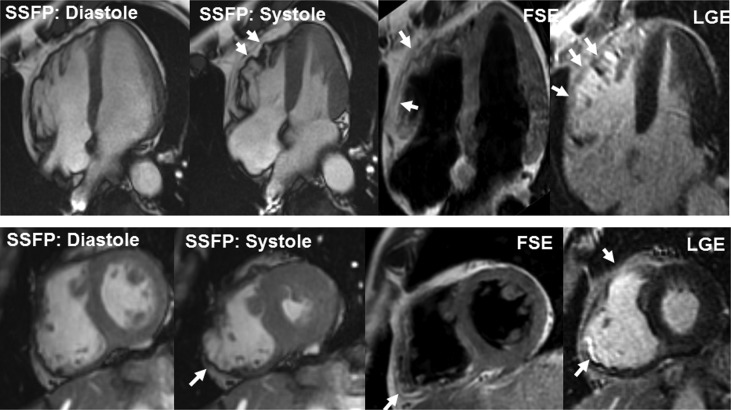
Using dedicated software (Mass 6.1; Medis Medical Imaging Systems, Leyden, The Netherlands), the following functional parameters were obtained from the short-axis images: right and left ventricular EDVi, right and left ESVi, LV mass index, and right and left ejection fraction (EF). The RV and LV volume indexes were compared with the respective reference values clustered for class age and gender. Furthermore, the ratio between RV and LV EDVi was quantified. The RV and LV WM were classified as normal WM, minor WM abnormalities (hypokinetic segment), or major WM abnormalities (akinetic or bulging segment; Figures 1 and 2 ).