Spontaneous coronary artery dissection (SCAD) is an increasingly recognized cause of myocardial infarction; however, the role of cardiac rehabilitation (CR) for patients with SCAD has not been well defined. To further understand CR in patients with SCAD, we studied a large cohort of patients with confirmed SCAD enrolled in the Mayo Clinic SCAD Registry from January 2010 to December 2014 (n = 354). Demographics, clinical characteristics, mental health status, and details about CR participation and experience were collected through medical record review and questionnaires. Participants at time of SCAD were 46 ± 10 years old; 96% were women. Most (76%) attended ≥1 CR sessions, averaging 18 ± 12 sessions. Most reported CR-related physical and emotional benefits (82% and 75%, respectively). Of the CR nonparticipants, 57 of 85 reported not participating because CR was not recommended by their health care provider. Other reasons included inadequate transportation (10 of 85), no insurance coverage (7 of 85), cost (2 of 85), no energy (2 of 85), being too ill (2 of 85), and miscellaneous comments (5 of 85). In conclusion, 3 of 4 of patients with SCAD participated in CR, most of whom reported benefit. Lack of recommendation for CR by a health care provider was the primary reason patients did not participate.
Despite cardiac rehabilitation (CR) being a class I, national guideline-recommended therapy that reduces morbidity/mortality and improves quality of life after acute myocardial infarction (AMI), CR services are vastly underutilized. Studies have shown that young, healthy women are less likely to be referred for CR, and when referred, they are less likely to attend. The benefit of CR has not been well studied in patients with spontaneous coronary artery dissection (SCAD), who are frequently otherwise healthy, previously fit young women. In addition, the association of SCAD with physical activity may raise concerns regarding safety of CR referral and treatment. However, a hypothesis-generating case series of 9 patients demonstrated that CR after SCAD AMI can improve aerobic capacity, body composition, and overall mental health without adverse events. We aimed to understand the role of CR in patients with SCAD in the Mayo Clinic SCAD Registry.
Methods
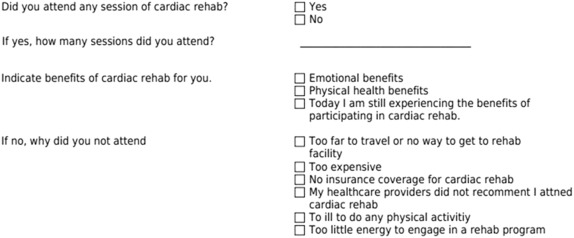
This study was approved by the Mayo Clinic Institutional Review Board, and written informed consent was obtained from each patient as part of the Mayo Clinic SCAD Registry. The Mayo Clinic SCAD Registry was created in response to an organized effort of an online community of patients with SCAD. Participants are recruited to the Mayo Clinic SCAD Registry through social media, the Mayo Clinic SCAD Research Program website and/or provider referral and are enrolled on coronary angiographic confirmation of the diagnosis by ≥2 interventional cardiologists. We reviewed 419 patients enrolled in the Mayo Clinic SCAD Registry from January 2010 to December 2014 of whom 354 had complete CR surveys. Patient data including demographics, socioeconomics, clinical characteristics, medical history, and current health status were obtained from a series of questionnaires including as follows: Generalized Anxiety Disorder 7-Item Scale (GAD-7), Patient Health Questionnaire-9 (PHQ-9), Rand 36 Items SF Health Survey (SF-36), Mayo Clinic Women Heart Clinic Risk Assessment, Mayo Clinic Women/Men with Heart Disease Survey, Mayo Clinic SCAD Questionnaire, and Mayo Clinic SCAD Supplemental Survey. In this patient population, indications for CR included AMI and/or percutaneous transluminal coronary intervention. Participation in CR was defined as attendance in ≥1 CR sessions. In addition to extensive clinical and mental health data, these questionnaires also included specific questions about the patient’s participation or lack thereof in CR including the level of attendance, barriers to attendance, and perceived emotional and physical benefits ( Figure 1 ).
Statistical analyses were performed using JMP statistical software, version 10.0.0 (SAS, Cary, North Carolina). Continuous variables are presented as mean ± SD. Categorical variables are presented as frequencies or percentages. Baseline characteristics were compared between CR participants and nonparticipants using a chi-square test for categorical variables and Wilcoxon rank-sum test for continuous variables. Univariate analyses were performed to determine the differences between baseline characteristics and outcomes according to CR participation status. All comparisons were 2-sided, and a p-value <0.05 was considered statistically significant.
Results
Of the 354 patients in our study, patients geographically represented 48 of 50 US states, Canada, Europe, Australia, and New Zealand. The mean age of participants at time of survey was 50 ± 10 years, and the mean age of participants at time of SCAD was 46 ± 10 years. Mean between time of surveys and time of SCAD events was 3.3 ± 4 years. Ninety-six percent of patients were women. After hospital dismissal, 269 patients (76%) participated in ≥1 CR sessions, and those users averaged 18 ± 12 sessions. One hundred seventy-eight subjects (66%) participated in >10 CR sessions. There were no notable differences between the CR participants versus nonparticipants at baseline except that participants were more likely to be taking aspirin and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and less likely to have a history of right coronary artery SCAD ( Table 1 ).
| Variables | Overall (n=354) | Cardiac Rehabilitation | P-value | |
|---|---|---|---|---|
| Yes (n=269) | No (n=85) | |||
| Age (years) at time of SCAD, mean ± SD | 45.6 ± 9.8 | 45.4 ± 9.9 | 46.6 ± 9.8 | 0.49 |
| Age (years) at time of survey, mean ± SD | 50.1 ± 9.6 | 49.9 ± 9.3 | 50.9 ± 10.6 | 0.48 |
| Female | 341 (96%) | 262 (97%) | 79 (93%) | 0.06 |
| White | 319 (95%) | 245 (91%) | 74 (87%) | 0.28 |
| Married | 296 (84%) | 222 (83%) | 74 (87%) | 0.33 |
| Living in own home/apartment | 344 (97%) | 260 (97%) | 84 (99%) | 0.29 |
| Yearly income >$50,000 | 300 (85%) | 223 (83%) | 77 (91%) | 0.09 |
| Yearly income >$80,000 | 234 (66%) | 172 (64%) | 62 (73%) | 0.13 |
| Employed full time | 184 (52%) | 139 (52%) | 45 (53%) | 0.84 |
| Employed part time | 60 (17%) | 51 (19%) | 9 (11%) | 0.07 |
| Completed 12 years of school | 348 (98%) | 263 (98%) | 85 (100%) | 0.16 |
| Completed 16 years of school | 245 (69%) | 189 (70%) | 56 (66%) | 0.45 |
| Body mass index, mean ± SD (kg/m 2 ) | 23.6 ± 7.1 | 23.5 ± 5.8 | 24.0 ± 10.3 | 0.64 |
| Hypertension | 90 (25%) | 65 (24%) | 25 (29%) | 0.33 |
| Diabetes mellitus | 9 (3%) | 6 (2%) | 3 (4%) | 0.51 |
| Hypercholesterolemia | 92 (38%) | 77 (41%) | 15 (31%) | 0.20 |
| Fibromuscular dysplasia | 49 (22%) | 41 (24%) | 8 (17%) | 0.29 |
| Migraines | 88 (37%) | 72 (38%) | 16 (33%) | 0.50 |
| Connective tissue disease | 13 (5%) | 9 (5%) | 4 (8%) | 0.35 |
| Former tobacco use | 96 (27%) | 76 (28%) | 20 (24%) | 0.39 |
| Non-smoker | 242 (68%) | 185 (69%) | 57 (67%) | 0.77 |
| Left ventricular ejection fraction at last follow up, mean ± SD (self-reported) | 52.0 ± 12.2 | 55.9 ± 10.6 | 57.8 ± 9.3 | 0.23 |
| Details of initial SCAD event (self-reported) | ||||
| Unstable angina pectoris | 35 (16%) | 25 (15%) | 10 (21%) | 0.32 |
| Non-ST segment elevation myocardial infarction | 125 (57%) | 94 (55%) | 31 (65%) | 0.25 |
| ST segment elevation myocardial infarction | 84 (38%) | 70 (41%) | 14 (29%) | 0.14 |
| Cardiac arrest | 16 (7%) | 14 (8%) | 2 (4%) | 0.34 |
| Ventricular arrhythmia | 17 (8%) | 15 (9%) | 2 (4%) | 0.29 |
| Medical treatment only | 98 (46%) | 71 (43%) | 27 (56%) | 0.09 |
| Thrombolysis | 22 (10%) | 19 (11%) | 3 (6%) | 0.53 |
| Coronary artery bypass grafting | 23 (11%) | 18 (11%) | 5 (10%) | 0.98 |
| Percutaneous coronary intervention | 102 (47%) | 85 (50%) | 17 (35%) | 0.07 |
| Coronary artery SCAD location (self-reported) | ||||
| Left main | 12 (5%) | 7 (4%) | 5 (10%) | 0.20 |
| Left anterior descending | 130 (60%) | 105 (61%) | 25 (53%) | 0.31 |
| Left circumflex | 33 (15%) | 25 (15%) | 8 (17%) | 0.71 |
| Right | 30 (14%) | 19 (11%) | 11 (23%) | 0.04 |
| Recurrent SCAD (self-reported) | 71 (21%) | 58 (22%) | 13 (16%) | 0.23 |
| Current medications | ||||
| Aspirin | 313 (93%) | 245 (91%) | 68 (81%) | 0.01 |
| Beta-blockers | 125 (35%) | 96 (36%) | 29 (34%) | 0.07 |
| Statin | 134 (38%) | 108 (40%) | 26 (31%) | 0.11 |
| Thienopyridine | 107 (30%) | 87 (32%) | 20 (22%) | 0.09 |
| Angiotension converting enzyme inhibitor/Angiotension receptor blocker | 78 (22%) | 67 (25%) | 11 (13%) | 0.02 |
Of those 269 patients who participated in CR, 82% perceived physical health benefits, 75% perceived emotional health benefits, and 45% reported still experiencing the benefits of participating in CR at the time of survey ( Figure 2 ). Of those 85 patients who did not participate in CR, the primary reason was because their health care provider did not recommend CR. Other barriers included inadequate transportation, no insurance coverage, cost, no energy, and being too ill to do any physical activities ( Figure 3 ).
Other reasons for limited or no participation was due to the CR programs not meeting the needs of several patients with SCAD who were considerably active and physically fit before their event. This concern was reflected by the following comments in the survey: “I found it too slow for me and left the program,” “it was a waste of my time,” “my own workout routine was more than the rehab program,” and “I tried going and did not think it was worthwhile.”
For the entire group, mean PHQ-9 and GAD-7 scores were 3.9 ± 3.6 and 4.7 ± 4.8, respectively, at a mean time of 2.8 ± 4.2 years between the survey date and initial SCAD event ( Table 2 ). On comparative analyses, the PHQ-9 scores were similar in the CR participants and nonparticipants. CR participants had slightly higher mean GAD-7 scores. Despite this, 37 CR participants and 11 nonparticipants had GAD-7 scores >10 (p = 0.45) suggesting similar rates of moderate or greater GAD among the 2 groups. Health-related quality of life as evaluated by the SF-36 was similar between CR participants and nonparticipants, including scores on physical functioning, general health, and vitality.
| Variables | Overall (n=354) | Cardiac Rehabilitation | P-value | |
|---|---|---|---|---|
| Yes (n=269) | No (n=85) | |||
| Time from SCAD to survey, mean ± SD (months) | 33.6 ± 50.6 | 33.4 ± 51.9 | 34.3 ± 46.5 | 0.81 |
| Generalized Anxiety Disorder 7 score, mean ± SD | 4.7 ± 4.8 | 4.9 ± 4.7 | 3.9 ± 4.9 | 0.03 |
| Patient Health Questionnaire 9 score, mean ± SD | 3.9 ± 3.6 | 4.0 ± 3.5 | 4.0 ± 3.8 | 0.71 |
| Rand 36 Items SF Health Survey subscales, mean ± SD | ||||
| Physical functioning | 80.5 ± 19.9 | 81.1 ± 18.7 | 78.4 ± 23.4 | 0.79 |
| Role functioning-physical | 63.8 ± 41.1 | 63.0 ± 41.5 | 66.5 ± 39.6 | 0.50 |
| Bodily pain | 55.5 ± 7.8 | 55.2 ± 7.5 | 56.5 ± 8.9 | 0.36 |
| General health | 65.6 ± 20.9 | 65.3 ± 20.8 | 66.2 ± 21.2 | 0.73 |
| Vitality | 51.9 ± 22.5 | 52.4 ± 22.5 | 50.6 ± 22.7 | 0.49 |
| Social functioning | 78.9 ± 24.3 | 78.8 ± 24.5 | 79.4 ± 23.8 | 0.87 |
| Role functioning-emotional | 78.2 ± 35.8 | 78.2 ± 36.0 | 78.0 ± 35.5 | 0.83 |
| Mental health | 73.7 ± 15.7 | 72.9 ± 16.0 | 76.3 ± 14.4 | 0.09 |
| Duration of aerobic exercise (minutes) | ||||
| Never | 45 (13%) | 26 (10%) | 19 (25%) | |
| <20 | 31 (9%) | 24 (9%) | 7 (9%) | |
| 20-30 | 89 (26%) | 69 (27%) | 20 (26%) | 0.01 |
| 30-60 | 147 (44%) | 119 (46%) | 28 (36%) | |
| >60 | 24 (7%) | 21 (8%) | 3 (4%) | |
| Frequency of aerobic exercise sessions/week | ||||
| Never | 50 (15%) | 28 (11%) | 22 (28%) | |
| <1 | 30 (9%) | 25 (10%) | 5 (6%) | |
| 1-2 | 66 (19%) | 55 (21%) | 11 (14%) | 0.002 |
| >3 | 195 (57%) | 154 (59%) | 41 (52%) | |
| Frequency of non-aerobic exercise/week (hours) | ||||
| <1 | 55 (16%) | 40 (16%) | 15 (20%) | |
| 1 | 51 (15%) | 41 (16%) | 10 (13%) | |
| 2 | 81 (24%) | 70 (27%) | 11 (14%) | 0.16 |
| 3 | 55 (16%) | 41 (16%) | 14 (18%) | |
| >4 | 92 (28%) | 66 (26%) | 26 (34%) | |
| Regularly do strength building exercises with resistance or weight lifting equipment | 105 (30%) | 86 (32%) | 19 (22%) | 0.09 |
| Reasons for not exercising | ||||
| Lack of appropriate facility or equipment | 21 (6%) | 16 (6%) | 5 (6%) | 0.98 |
| No one to exercise with | 37 (10%) | 28 (10%) | 9 (11%) | 0.96 |
| Physically unable to exercise | 36 (10%) | 25 (9%) | 11 (13%) | 0.33 |
| Not enough time | 147 (42%) | 119 (44%) | 28 (33%) | 0.07 |
| Don’t like exercise | 49 (14%) | 38 (14%) | 11 (13%) | 0.78 |
| Lack of motivation | 89 (25%) | 69 (26%) | 20 (24%) | 0.69 |
| Cost | 22 (6%) | 18 (7%) | 4 (5%) | 0.51 |
| Other reasons | 40 (11%) | 28 (10%) | 12 (14%) | 0.35 |
| No reason | 88 (25%) | 70 (26%) | 18 (21%) | 0.37 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


