Recurrent pericarditis (RP) affects 10% to 50% of patients with acute pericarditis. The use of steroids has been associated with increased recurrence rate of pericarditis, along with known major side effects. Cardiac magnetic resonance imaging (CMR) is more frequently used to assess pericardial inflammation and less commonly to guide therapy. The aim of this study was to assess the utility of CMR in the management of RP compared with standard therapy. A total of 507 consecutive patients with RP after the first attack, all of whom were treated with colchicine and nonsteroidal anti-inflammatory drugs as first-line therapy, were retrospectively evaluated. There were 257 patients who were treated with medications and received CMR-guided therapy (group 1) and 250 patients who were treated with medications without CMR (group 2). The 2 groups had similar baseline characteristics and follow-up periods (17 ± 7.9 vs 16.3 ± 16.2 months, respectively, p = 0.97). CMR was used to assess the presence of pericardial inflammation, and on the basis of the results, the clinician made changes to the steroid dose dictated by the severity of inflammation. There was no significant difference in the incidence of constrictive pericarditis, pericardial window, or pericardiectomy between groups during the follow-up. However, group 2 patients had a larger number of steroid pulse therapies (defined as prednisone 50 mg/day orally for 10 days and tapering to none over 4 weeks), and higher overall total milligrams of steroid administered compared with the CMR group (p = 0.003 and p = 0.001, respectively). Recurrence and pericardiocentesis rates were lower in group 1 (p <0.0001). In conclusion, CMR-guided therapy modulates the management of RP. This approach decreased pericarditis recurrence and exposure to steroids.
Recurrent pericarditis (RP) is one of the most challenging complications of pericarditis, affecting 20% to 30% of patients after the first attack of pericarditis. It is associated with high health care costs due to recurrent admissions for chest pain and heart failure symptoms. In few cases, RP may progress to constrictive pericarditis with need for pericardiectomy. Nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine are considered the first-line therapeutic agents for use in patients with RP. Steroids are often used prematurely in the course of the disease, without allowing enough time for standard anti-inflammatory medications to take effect. Cardiac magnetic resonance imaging (CMR) allows the direct measurement of pericardial thickness and assessment of inflammation, edema, and constrictive physiology. CMR with late gadolinium enhancement (LGE) of pericardium suggests active inflammation and correlates well with histopathologic findings. Although this technology has been available for quite some time, its utility in a cohort of patients with RP has not been previously reported. We hypothesized that the use of CMR with LGE has an impact on therapeutic decisions in patients with RP and thus affects clinical outcomes in this condition.
Methods
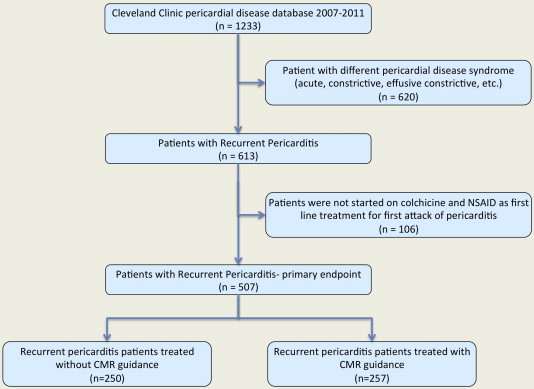
We retrospectively identified 507 consecutive patients with RP from 2007 to 2011 in the Cleveland Clinic’s Center for Pericardial Disease database. RP was defined as recurrence of pericarditis <6 weeks after weaning of anti-inflammatory medications. This definition was based on the European Society of Cardiology guidelines on the diagnosis and management of pericardial diseases, published in 2004.
All patients ≥18 years of age who developed recurrence of pericarditis symptoms after the first attack of pericarditis were included in the study. All patients were treated initially with colchicine and NSAID as the first-line therapy and started on steroids after the first recurrence. Patients who were not started on colchicine and NSAID as first-line therapy or treated with steroids at the initial diagnosis were excluded from the study (n = 106; Figure 1 ). Patients were then stratified as those who did not undergo CMR during the course of treatment (group 1) and those who did (group 2). All patients were treated with standard therapy on the basis of the European Society of Cardiology guidelines and most recently published studies related to RP.
The decision to order CMR was at the discretion of the treating cardiologist. Patients with RP who were seen in the pericardial disease center clinic were subject to CMR compared with patients seen in general cardiology clinic. CMR studies with LGE were performed using a standard protocol, as previously described in detail and interpreted by level III trained and certified cardiologists. In summary, a comprehensive pericardial CMR protocol should include morphologic evaluation of the cardiac chambers, pericardium, and mediastinum using fast spin-echo T1-weighted sequences with black-blood preparation; assessment of global and regional systolic function of the left and right ventricles, using cine steady-state free precession sequences; depiction of pericardial fluid and/or edema using T2-weighted spin-echo imaging, preferably by using short-tau inversion-recovery sequences; ventricular coupling using real-time free-breathing cine sequences; and tissue characterization using LGE inversion-recovery CMR. All patients with initial CMR had ≥2 sequential studies to follow disease activity and response to treatment. LGE changes with subsequent studies were assessed to confirm inflammation activity and changes of LGE in response to treatment intervention. During acute inflammation, T2-weighted short-tau inversion recovery imaging detects fluid and/or edema of the inflamed pericardial layers, and delayed enhancement imaging further shows brighter signal of inflamed pericardium. Decreased pericardial edema, brightness, and thickness were qualitatively used as parameters for response to medical therapy ( Figure 2 ).

There were several primary end points of interest: total number of milligrams of steroid used over the course of the disease, number of steroid pulse therapies, number of recurrences, and complications (constrictive pericarditis, pericardial windows, pericardiocentesis, pericardiectomy, and all-cause mortality). Steroid pulse therapy was defined as prednisone ≥50 mg administered orally daily for 10 days then tapered to none over a 4-week period.
Descriptive analyses were performed examining selected variables for each group. Continuous variables are expressed as mean ± SD or median (interquartile range) and were compared using unpaired Student’s t tests or Wilcoxon’s rank tests as appropriate. Categorical variable are expressed as number (percentage) and were compared using Pearson’s chi-square tests or Fisher’s exact tests as appropriate. Linear regression modeling was performed to assess the independent predictors of number of steroid pulses. The model was adjusted for baseline demographics, co-morbidities, history of recurrence, and CMR. A p value <0.05 was set a priori and considered statistically significant. All statistical analyses were performed using SPSS version 19 for Windows (SPSS, Inc., Chicago, Illinois). The study was approved by the institutional review board with waiver of the requirement for informed consent and complied with the Declaration of Helsinki.
Results
The study cohort consisted of 507 patients (mean age 48 ± 14 years, 50.2% men) who met the inclusion criteria with the diagnosis of RP ( Figure 1 ). All patients were treated initially with colchicine and NSAIDs followed by oral steroids and continued for the whole treatment period ( Table 1 ). Almost half of the cohort received CMR-guided therapy. There were no contraindications to CMR in either group (i.e., acute or chronic renal failure, allergy to gadolinium contrast). Furthermore, there were no significant differences in demographics, baseline co-morbidities, cause of disease, and medication use between the groups ( Table 1 ). The 2 groups had similar follow-up periods (mean 17 ± 7.9 vs 16.3 ± 6.2 months, p = 0.97).
| Variable | Managed With Cardiac Magnetic Resonance Imaging | P | |
|---|---|---|---|
| Yes (n = 257) | No (n = 250) | ||
| Mean age (SD), years | 47±13 | 48±14 | 0.84 |
| Men | 123 (47.9%) | 132 (52.8%) | 0.28 |
| White | 123 (48%) | 130 (52%) | 0.37 |
| Mean follow-up (SD), (months) | 17±8 | 16.3±6.2 | 0.97 |
| Number of follow-up | 9 | 9 | 1.0 |
| Hypertension | 94 (36.6%) | 91(36.4%) | 1.0 |
| Diabetes Mellitus | 17 (6.6%) | 20 (8%) | 0.61 |
| Coronary artery disease | 21 (8.2%) | 19 (7.6%) | 0.87 |
| Heart failure | 8 (3.1) | 7 (2.8) | 1.0 |
| Valvular heart disease | 53 (20.6) | 40 (16) | 0.20 |
| Atrial Fibrillation | 23 (8.9%) | 24 (9.6%) | 0.87 |
| Etiology of Pericarditis | |||
| Idiopathic | 181 (70.4%) | 180 (72%) | 0.76 |
| Post-pericardiotomy syndrome | 29 (11.3%) | 25 (10%) | 0.66 |
| Other (viral, autoimmune, uremia) | 47 (18%) | 45 (18%) | 1.0 |
| Medications | |||
| Colchicine | 257 (100%) | 250 (100%) | 1.0 |
| NSAID (ibuprofen) | 257 (100%) | 250 (100%) | 1.0 |
| Aspirin | 31 (12%) | 23 (9.2%) | 0.31 |
| Statin use | 89 (34.6%) | 81 (32.4%) | 0.63 |
| Steroids dose 1mg/kg/day | 189 (73.5%) | 205 (82%) | 0.02 |
| Steroids dose 0.5mg/kg/day | 68 (26.4%) | 45 (18%) | 0.03 |
After a mean follow-up time of 17 months, patients who had no CMR done (group 2) had a larger number of steroid pulse therapies (2.41 ± 1.06 vs 0.63 ± 0.91, p = 0.0001) and higher overall total milligrams of steroid administered (1,695.4 ± 1,166.09 vs 486 ± 546.4, p = 0.0001) compared with those who received CMR-guided therapy (group 1). Furthermore, patients in group 2 had more recurrence of symptoms (p = 0.001) and pericardiocentesis (p = 0.001) ( Table 2 ). There was no significant difference in the occurrence of pericardial window, constrictive pericarditis, pericardiectomy, or death between the groups. The duration of therapy needed for complete resolution of recurrence (freedom from disease) was 6 ± 2.1 months in group 1 compared with 13 ± 3.2 months in group 2 (p = 0.001).
| Variable | Managed With Cardiac Magnetic Resonance Imaging | P | |
|---|---|---|---|
| Yes (n = 257) | No (n = 250) | ||
| Mean WSR (SD), (mm/hr) | 32.0±27.2 | 32.3±27.9 | 0.89 |
| Number of prednisone pulses (SD) | 0.63±0.91 | 2.41±1.06 | <0.0001 |
| Total prednisone (SD), (mg) | 486±546 | 1695.4±1166 | <0.0001 |
| Number of recurrences, (SD) | 1.19±1.2 | 3.6±2.18 | <0.0001 |
| Mean glycated hemoglobin, HbA1c, (SD)(%) | 7.4±0.6 | 9.3±1.2 | <0.0001 |
| Constrictive pericarditis | 19 (7.4%) | 17 (6.8%) | 0.86 |
| Pericardiocentesis | 15 (5.8%) | 40 (16%) | <0.0001 |
| Pericardial Window | 56 (21.8%) | 44 (17.6%) | 0.26 |
| Pericardiectomy | 12 (4.7) | 14 (5.6) | 0.69 |
| Death | 1 (0.4%) | 2 (0.8%) | 0.61 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


