B-type natriuretic peptide (BNP) has been shown to predict outcomes after conventional aortic valve replacement. The aim of the present study was to investigate whether BNP also predicts the outcomes after transcatheter aortic valve implantation (TAVI). A total of 58 patients (36 men, age 84 ± 5 years) underwent TAVI in our institution for severe aortic stenosis (aortic valve area 0.6 ± 0.1 cm 2 , mean gradient 41 ± 15 mm Hg) at high risk of surgery (logistic European System for Cardiac Operative Risk Evaluation 34 ± 17%). BNP was measured before and 24 hours after TAVI. The 30-day survival rate was 91%. Although the baseline clinical and hemodynamic characteristics were similar among the 30-day survivors (n = 53) and nonsurvivors (n = 5), the BNP levels were significantly lower in the 30-day survivors, at both baseline (463 ± 265 vs 1,067 ± 655 pg/ml; p = 0.005) and 24 hours after TAVI (488 ± 238 vs 1,632 ± 1,028 pg/ml; p <0.0001). The BNP levels were significantly greater in patients experiencing one major adverse event at 30 days. On multivariate analysis, only BNP levels (baseline value and change at 24 hours) were independent predictors of 30-day survival. Kaplan-Meier analysis showed that 30-day survival was significantly lower in patients with than in those without both a baseline BNP level >428 mg/dl (p = 0.04) and a significant BNP increase of >170 pg/ml at 24 hours after TAVI (p = 0.001). In conclusion, BNP is a strong predictor of 30-day outcomes after transcatheter aortic valve implantation, at both baseline and 24 hours after the procedure.
Transcatheter aortic valve implantation (TAVI) has recently been developed to treat patients with severe aortic stenosis and considered at high risk of surgery. Usually, candidates for TAVI are octogenerians with several co-morbidities (i.e., renal failure, chronic obstructive pulmonary disease, previous stroke, pulmonary hypertension) and severe heart failure. Despite the minimally invasive aspect of the technique, the periprocedural complications and mortality have remained high and have not been precisely predicted by the European System for Cardiac Operative Risk Evaluation (EuroSCORE). In patients undergoing conventional aortic valve replacement, the perioperative outcome has been more accurately predicted by the B-type natriuretic peptide (BNP) level than by the EuroSCORE. The present study evaluated whether BNP also predicts the outcomes for patients who undergo TAVI.
Methods
From January 2008 to December 2009, 59 patients who had undergone TAVI at our institution using the Edwards Sapien valve (Edwards Lifesciences, Irvine, California), were consecutively and prospectively enrolled in the present study. Patients with severe calcific aortic stenosis (aortic valve area <1 cm 2 and/or peak transvalvular velocity >4 m/s) were considered at high risk of a conventional aortic valve replacement (logistic EuroSCORE >20% or Society of Thoracic Surgeons score >10%) or had a contraindication for surgery. The exclusion criteria for TAVI using the Edwards Sapien valve included congenital or noncalcified aortic stenosis, an unprotected left main lesion, coagulation disorder, endocarditis, recent myocardial infarction or stroke (within 1 month), aortic annulus diameter <18 or >25 mm, and left ventricular ejection fraction <20%. One patient was excluded from the present study because he had undergone TAVI in the absence of significant aortic stenosis to treat severe aortic regurgitation due to a degenerated bioprosthesis (valve-in-a-valve procedure). Therefore, the final population constituted 58 patients. Our local ethics committee approved the protocol.
Blood was drawn from an antecubital vein into chilled ethylenediaminetetraacetic acid tubes, and the serum BNP level was determined using the fluorescent immunoassay (Triage BNP Test, Biosite Diagnostics, San Diego, California). The assay analytic sensitivity was 5 pg/ml. The measuring range was 5 to 5,000 pg/ml, with a precision of 8.8%. Blood samples were obtained at baseline and 24 hours after TAVI. Patient survival was determined from reviews of the medical records or direct patient contact in December 2009.
The data are presented as the mean ± SD, unless otherwise stated. Differences between patient groups were analyzed using Student’s t test for continuous variables or the chi-square test for categorical variables. The receiver operating characteristic curve was determined to evaluate the performance of BNP to predict survival. The optimal cutoff points for the serum BNP levels were chosen when the sensitivity and specificity were maximized. Survival curves according to the BNP level were established using the Kaplan-Meier estimation method. Multivariate analysis of the predictive factors of death was performed using the Cox proportional hazards method. A p value <0.05 was considered statistically significant. Analyses were performed using XLSTAT software, version Pro2009 for Windows (Addinsoft, France).
Results
The patient characteristics are listed in Table 1 . Of the 58 patients, 34 underwent Sapien valve implantation using a transfemoral and 24 patients using a transapical approach. No significant differences were found in the baseline characteristics between the groups in terms of aortic stenosis severity, left ventricular function, logistic EuroSCORE, presence of coronary artery disease, or chronic pulmonary insufficiency. Patients treated by a transapical approach were significantly younger and more frequently had peripheral vascular disease but were less often affected by pulmonary hypertension than those who underwent transfemoral TAVI. The baseline characteristics were similar between the 30-day survivors and nonsurvivors.
| Variable | All Patients (n = 58) | Transfemoral (n = 34) | Transapical (n = 24) | 30-Day Survivors (n = 53) | 30-Day Nonsurvivors (n = 5) |
|---|---|---|---|---|---|
| Age (years) | 84 ± 5 | 85 ± 4 | 82 ± 4 ⁎ | 84 ± 4 | 85 ± 6 |
| Gender (male/female) | 36/22 | 20/14 | 16/8 | 32/21 | 4/1 |
| Aortic valve area (cm 2 ) | 0.6 ± 0.1 | 0.6 ± 0.1 | 0.6 ± 0.1 | 0.6 ± 0.1 | 0.5 ± 0.1 |
| Mean gradient (mm Hg) | 41 ± 15 | 40 ± 14 | 42 ± 10 | 41 ± 14 | 39 ± 20 |
| Left ventricular ejection fraction (%) | 47 ± 15 | 45 ± 15 | 49 ± 14 | 47 ± 15 | 45 ± 16 |
| Logistic European System for Cardiac Operative Risk Evaluation (%) | 34 ± 17 | 33 ± 16 | 35 ± 18 | 34 ± 17 | 37 ± 18 |
| Coronary artery disease | 40 (69%) | 21 (62%) | 19 (79%) | 36 (68%) | 4 (80%) |
| Peripheral vascular disease | 36 (62%) | 16 (47%) | 20 (83%) ⁎ | 33 (62%) | 3 (60%) |
| Pulmonary hypertension | 16 (27%) | 15 (44%) | 1 (4%) ⁎ | 14 (26%) | 2 (40%) |
| Chronic obstructive pulmonary disease | 15 (26%) | 8 (23%) | 7 (29%) | 13 (24%) | 2 (40%) |
⁎ p <0.05 for comparison between transapical and transfemoral groups.
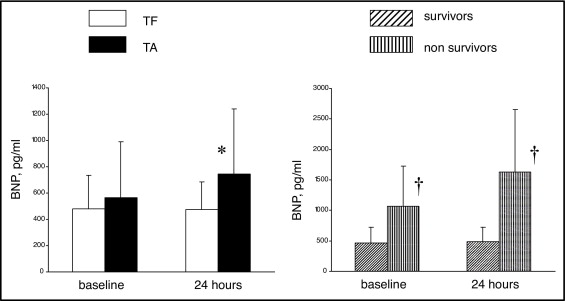
The results are listed in Table 2 . At baseline, the BNP serum levels were similar between the transfemoral and transapical groups but were significantly greater in the 30-day nonsurvivors than in the 30-day survivors (1,067 ± 655 vs 463 ± 265 pg/ml, p = 0.005). At 24 hours, the BNP level had significantly increased after transapical TAVI but had not after transfemoral TAVI (+183 ± 324 vs −7 ± 148 pg/ml, respectively; p = 0.01). The change in BNP level at 24 hours after TAVI was significantly greater in the nonsurvivor group than in the survivor group (566 ± 408 vs 25 ± 169 pg/ml; p <0.0001). At 24 hours, the serum BNP levels (586 ± 342 pg/ml) correlated well with troponin I peak (4.6 ± 6.4 ng/ml; r = 0.70) and creatine kinase-MB peak (17 ± 18 μg/L; r = 0.61). Figure 1 shows the BNP serum levels at baseline and 24 hours after TAVI in the different groups of patients.
| B-Type Natriuretic Peptide (ng/ml) | All Patients (n = 58) | Transfemoral (n = 34) | Transapical (n = 24) | 30-Day Survivors (n = 53) | 30-Day Nonsurvivors (n = 5) |
|---|---|---|---|---|---|
| Baseline | 515 ± 326 | 481 ± 253 | 563 ± 428 | 463 ± 265 | 1,067 ± 655 † |
| At 24 hours | 586 ± 342 | 473 ± 211 | 747 ± 493 ⁎ | 488 ± 238 | 1,632 ± 1,028 † |
| Increase at 24 hours | 71 ± 216 | −7 ± 148 | 183 ± 324 ⁎ | 25 ± 169 | 566 ± 408 † |
⁎ p <0.05 for comparison between transapical and transfemoral groups.
† p <0.05 for comparison between survivors and nonsurvivors.
The overall 30-day survival rate was 91% (94% in the transfemoral group and 87% in the transapical group). The cause of death in the transapical group was refractory heart failure in 2 patients and fatal hemothorax after pacemaker implantation in 1 patient. In the transfemoral group, 1 patient died from traumatic cerebral hemorrhage after falling and 1 patient died from heparin-induced thrombocytopenia syndrome. On multivariate analysis, only the BNP levels (baseline value and change at 24 hours) were independent predictors of 30-day mortality ( Table 3 ). The receiver operating characteristic analysis ( Figure 2 ) showed that the optimal cutoff value of the baseline BNP serum level to predict 30-day survival was 428 pg/ml, with a sensitivity of 80% and specificity of 64%. The area under the curve was 0.71.
| Variable | HR (95% CI) | p Value |
|---|---|---|
| Univariate analysis | ||
| Change in B-type natriuretic peptide at 24 hours | 1.005 (1.002–1.008) | 0.001 |
| Baseline B-type natriuretic peptide | 1.001 (1.000–1.002) | 0.002 |
| Peripheral vascular disease | 1.490 (0.249–8.919) | 0.66 |
| Pulmonary hypertension | 1.541 (0.257–9.224) | 0.63 |
| Age | 1.047 (0.849–1.291) | 0.66 |
| Left ventricular ejection fraction | 0.974 (0.919–1.033) | 0.38 |
| Peak troponin | 1.192 (1.065–1.333) | 0.04 |
| Logistic European System for Cardiac Operative Risk Evaluation | 1.012 (0.962–1.064) | 0.64 |
| Multivariate analysis | ||
| Baseline B-type natriuretic peptide | 1.001 (1.000–1.0002) | 0.01 |
| Change in B-type natriuretic peptide at 24 hours | 1.006 (1.002–1.0009) | 0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


