Mitral annular calcium and aortic valve sclerosis on transthoracic echocardiography (TTE) are independently associated with cardiovascular (CV) events in patients with coronary artery disease (CAD). However, the prognostic value of calcific deposits at multiple sites is unknown. We performed TTEs in a prospective cohort of 595 outpatients with stable CAD and graded the severity of calcific deposition at 6 sites: mitral annulus, aortic valve, aortic ring, sinotubular junction, papillary muscle tip, and left main coronary artery. For each site with moderate calcific deposition or greater, 1 point was given to generate a composite cardiac calcium score (maximum of 6). The primary end point was the occurrence of CV events—a composite of death, myocardial infarction, stroke, transient ischemic attack, and heart failure. The association of the composite calcium score with CV events was evaluated using multivariate Cox proportional hazards models. Over a median follow-up of 4.2 years, 205 CV events occurred. Participants with a composite calcium score ≥2 had a higher risk of CV events (11.1 events/100 person-years) than those with a score of 0 (5.5 events/100 person-years, unadjusted hazard ratio [HR] 2.01, p <0.001), but this association was not significant after multivariate adjustment. The risk of death was higher in participants with a composite calcium score of ≥2 (8.9 events/100 person-years) versus those with a score of 0 (3.6 events/100 person-years, unadjusted HR 2.51, p <0.001). After adjustment for age, diabetes mellitus, previous coronary revascularization, diastolic blood pressure, estimated glomerular filtration rate, and serum phosphorus level, the risk of death remained higher in participants with a composite calcium score of ≥2 compared with those with a score of 0 (adjusted HR 1.76, 95% confidence interval 1.10 to 2.81, p = 0.02). In conclusion, a simple TTE-derived composite cardiac calcium score was independently predictive of death in patients with pre-existing CAD.
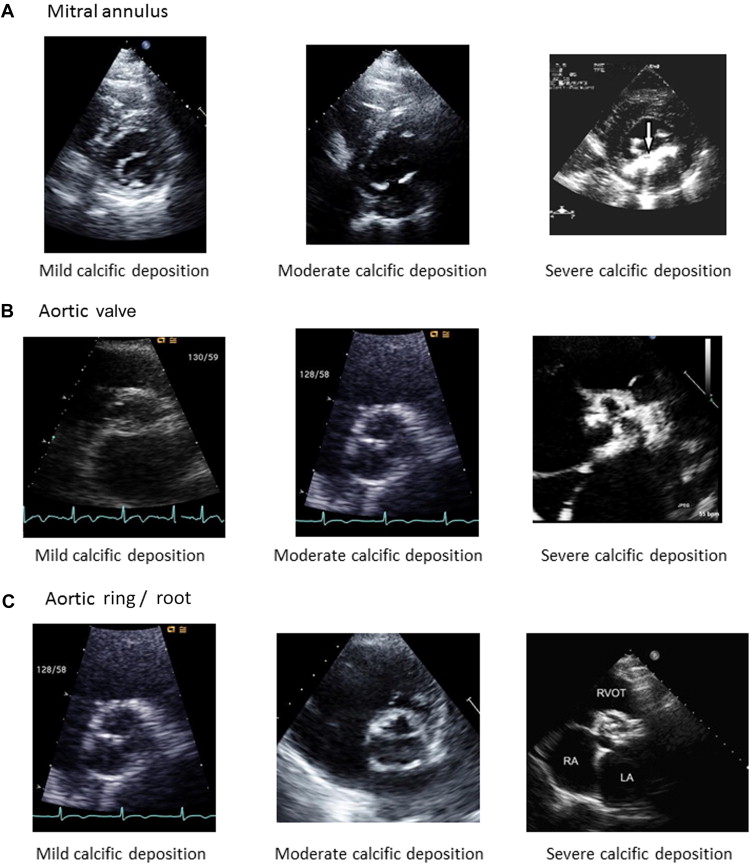
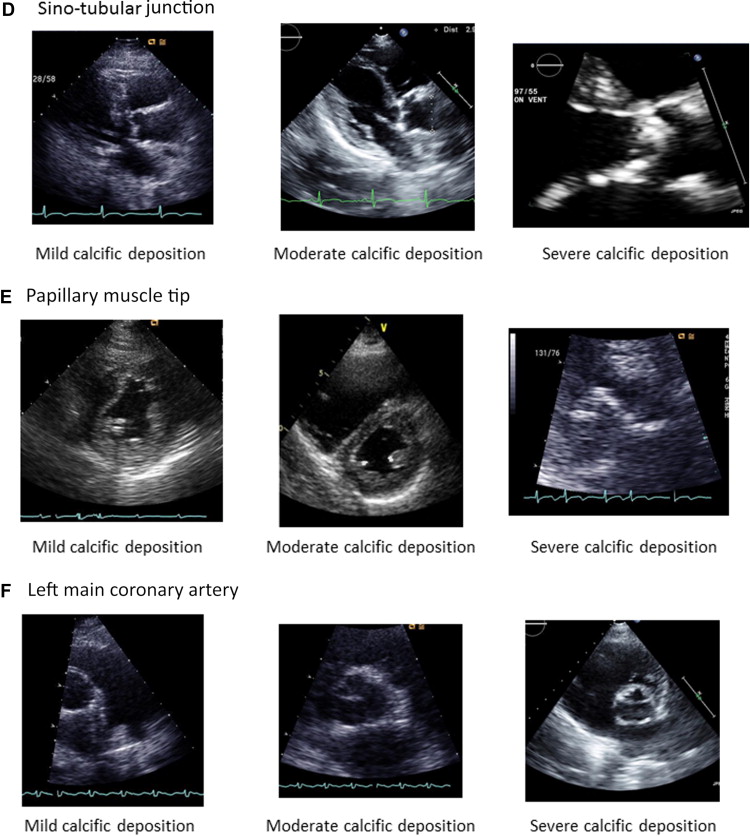
The presence of calcium deposits in the cardiovascular (CV) system has been associated with the presence of atherosclerotic disease in autopsy studies and population-based cohort studies. Two-dimensional (2D) transthoracic echocardiography (TTE) is able to detect calcific deposits at several discrete sites within the heart, epicardial coronary arteries, and great vessels. Other imaging techniques such as transesophageal echocardiography (TEE) and cardiac computed tomography (CT) to study cardiac calcification are limited because of the invasive nature and anesthetic and procedural risks in the case of TEEs and exposure to ionizing radiation and high cost in the case of CT. Mitral annular calcification (MAC) is associated with CV events, cardiac mortality, and all-cause mortality independent of traditional CV risk factors. Similarly, aortic valve sclerosis is associated with the presence of coronary artery disease (CAD) and elevated risk of CV morbidity and mortality. TTE studies enable detection of calcific deposits at other sites, including the aortic root, sinotubular junction, tips of the papillary muscles, and the proximal coronary arteries. In the present study, we developed a composite cardiac calcium score that grades the presence and severity of calcific deposition at 6 discrete sites as seen on conventional 2D TTE. The 6 sites chosen to develop this composite cardiac calcium score are mitral valve annulus, aortic valve annulus, aortic ring/root (defined as the portion between the aortic valve annulus and the sinuses of Valsalva), sinotubular junction, papillary muscle tip, and left main coronary artery. We then estimated the prognostic value of this composite cardiac calcium score for the prediction of CV events in patients with established CAD enrolled in the Heart and Soul Study.
Methods
The Heart and Soul Study is a prospective cohort study of outpatients with stable CAD.
The enrollment process for the Heart and Soul Study has been previously described. We used administrative databases to identify outpatients with documented CAD at 2 departments of the Veterans Affairs (San Francisco and Palo Alto, California), the University of California, San Francisco, and 9 public health clinics from the Community Health Network of San Francisco.
Participants were eligible to participate if they met 1 of the following : history of myocardial infarction, angiographic evidence of ≥50% stenosis by area in ≥1 coronary vessel, evidence of exercise-induced ischemia by treadmill electrocardiogram or stress nuclear perfusion imaging, history of coronary revascularization, or a previous diagnosis of CAD by an internist or a cardiologist. Subjects were excluded if they had a myocardial infarction within the previous 6 months, deemed themselves unable to walk 1 block, or were planning to move out of the local area within 3 years. From September 2000 to December 2002, 1,024 study participants provided informed consent and completed baseline echocardiographic and laboratory testing. This included 549 subjects (54%) with a history of myocardial infarction, 237 (23%) with a history of revascularization but not myocardial infarction, and 238 (23%) with a diagnosis of CAD that was documented by their physician (based on a positive angiogram or treadmill test in 98% of cases). The institutional review board at each enrolling center approved the study protocol, and all participants provided written informed consent.
Of the 1,024 participants who completed the baseline examination, a total of 595 participants underwent a repeat echocardiographic examination 5 years after enrollment, comprising the analytical cohort for this study. At the 5-year follow-up visit, the 595 participants completed an examination that included an interview, fasting blood draw, questionnaire, and TTE. A complete 2D TTE at rest was obtained in all patients using an Acuson Sequoia Ultrasound System and a 3.5-MHz transducer (Siemens Medical Solutions, Mountain View, California). All standard views were obtained during quiet respiration. Two highly experienced sonographers made all sonographic measurements, and a single, blinded cardiologist reader (NBS) evaluated, confirmed, and, when needed, corrected each measurement. In addition, the presence and severity of calcific deposition was measured at a total of 6 sites in the heart, using a predefined scoring system described in Table 1 and illustrated in Figure 1 . For each site with moderate or severe calcific deposition as defined earlier, the participant received 1 point, allowing for a composite calcium score ranging from 0 to 6. The composite calcium score was computed by a single cardiologist reader (NBS), who was blinded to the participants’ baseline clinical and laboratory information and did not participate in the adjudication of clinical outcomes. Age, gender, race, and medical history were determined by self-report. Study personnel measured height, weight, and blood pressure. Fasting blood samples were obtained to measure serum calcium, phosphorus, creatinine, cystatin C, C-reactive protein, total cholesterol, HDL cholesterol, LDL cholesterol, and triglyceride levels. Estimated glomerular filtration rate was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine-cystatin C equation.
| Site (Views) | Severity of calcific deposition | ||
|---|---|---|---|
| Mild | Moderate | Severe | |
| Mitral annulus (PSAX) | Calcific deposits limited to postero-medial terminus of posterior mitral annulus | Non-contiguous calcific deposits on the postero-medial and antero-lateral termini of the posterior mitral annulus | Contiguous calcific deposits extending from the lateral to medial termini of the posterior mitral annulus |
| Aortic valve (PLAX, PSAX) | Focal calcific deposits on one or more leaflets without leaflet restriction | Non-contiguous calcific deposits on one or more leaflets with no restriction or mild restriction | Contiguous calcific deposits on one or more leaflets with any degree of leaflet restriction |
| Aortic Root (PSAX) | Calcific deposits limited to anterior or posterior border of the aortic ring | Non-contiguous calcific deposits on both anterior and posterior borders of the aortic ring | Contiguous calcific deposits of the entire aortic ring (circumferential involvement) |
| Sino-tubular junction (PLAX) | Focal calcific deposits on one or both sino-tubular junctions | Calcific deposits on both sino-tubular junctions with no intrusion into the aortic lumen | Calcific deposits on both sino-tubular junctions with no intrusion into the aortic lumen |
| Papillary muscle tip (PSAX, A2C, A4C) | Calcific deposits on one (usually postero-medial) papillary muscle tip | Calcific deposits on both papillary muscle tips but not extending into the chordal apparatus | Calcific deposits on both papillary muscle tips with extension into the chordal apparatus |
| Left main coronary artery (PSAX, PLAX) | Focal calcific deposits on one or both walls of the left main coronary artery | Linear, non-contiguous involvement of <1 cm of one or both walls | Linear, contiguous involvement of >1 cm of both walls |
Annual telephone interviews were conducted with study participants (or their proxy) to inquire about interval emergency department visits, hospitalizations, or death. For any reported event, medical records, electrocardiograms, and if relevant, death certificates, autopsy reports, and coroner’s reports were retrieved. Clinical end point events were adjudicated by 2 independent, blinded investigators according to the prespecified criteria. In the event of disagreement, the adjudicators conferred, reconsidered their classification, and requested consultation from a third blinded adjudicator (MAW) as necessary. The occurrence of death and cause of death were verified by review of death certificates and relevant medical records. Myocardial infarction was defined using standard diagnostic criteria. Stroke was defined as a new neurologic deficit not known to be secondary to brain trauma, tumor, infection, or other cause. Transient ischemic attack was defined as a focal neurologic deficit (in the absence of head trauma) lasting >30 seconds and ≤24 hours, with rapid evolution of symptoms to the maximal level of deficit in <5 minutes and with subsequent complete resolution. Hospitalization for heart failure was defined as a minimum 1-night hospital stay with new or worsening signs and symptoms of heart failure.
For descriptive purposes, we divided participants into 3 groups based on the composite cardiac calcium score: subjects with no significant calcific deposition (composite calcium score of 0), with moderate or severe calcific deposition at 1 of the 6 sites (composite calcium score of 1), and with moderate or severe calcific deposition at 2 or more sites (composite calcium score of ≥2). To compare the differences among groups, we used the chi-square test for categorical variables and the 1-way ANOVA for continuous variables.
The primary outcome of this study was the occurrence of CV events, which included death, myocardial infarction, stroke, transient ischemic attack, and hospitalization for heart failure. We calculated event rates per 100 person-years categorized by the composite calcium score for the primary outcome and each of its components. Event rates by composite calcium score were compared using Cox proportional hazards regression models. Univariate analyses were performed to determine which clinical variables were independently associated with the composite calcium score. Adjustment for these covariates was performed using multivariate Cox proportional hazards models to estimate the association of the composite calcium score with the primary outcome and the individual clinical end points. Statistical significance was defined as a 2-sided p value <0.05. Results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). All analyses were performed using commercially available software (Stata 12; StataCorp LP, College Station, Texas).
Results
A total of 595 participants were included in the analysis. Moderate or severe calcific deposit was observed in the aortic valve in 147 participants (prevalence of 29.3%), followed by the aortic root (125 participants, prevalence of 23.8%) and the left main coronary artery (66 participants, prevalence of 12.4%). Moderate or severe calcific deposits on the mitral annulus were seen in 64 participants (prevalence of 10.8%). A total of 307 participants had a composite calcium score of 0, 176 had a score of 1, and 111 participants had a composite calcium score of 2 to 5. None of the participants in this study had a composite calcium score of 6. The distribution of moderate or severe calcific deposition at the various sites is summarized in Table 2 .
| Site | Number of participants with moderate or severe calcific deposition (N, %) |
|---|---|
| Aortic Valve | 147 (29.3%) |
| Aortic Root | 125 (23.8%) |
| Sino-tubular Junction | 66 (11.3%) |
| Left Main Coronary Artery | 67 (12.4%) |
| Mitral Annulus | 64 (10.8%) |
| Papillary Muscle Tip | 34 (5.4%) |
Compared with participants with a composite calcium score of 0, those with a score of ≥2 were older and had a higher proportion with a history of diabetes mellitus or coronary revascularization. The proportion of participants with previous myocardial infarction, heart failure, stroke, or peripheral arterial disease did not differ significantly between groups. Participants with calcific deposits at multiple sites also had higher diastolic blood pressure, reduced renal function, and higher serum phosphorus levels. There were, however, no significant differences between the groups in the fasting cholesterol profiles or C-reactive protein levels at baseline. The baseline demographic characteristics of the population studied are summarized in Table 3 .
| Composite cardiac calcium score | p-value | |||
|---|---|---|---|---|
| 0 | 1 | 2-5 | ||
| Number of patients | 307 | 176 | 111 | |
| Age (years) | 68.4 ± 9.9 | 73.1 ± 9.2 | 75.4 ± 9.4 | <0.001 |
| Male sex | 253 (82.4%) | 145 (82.4%) | 96 (86.5%) | 0.58 |
| Caucasian race | 173 (56.4%) | 105 (59.7%) | 73 (65.8%) | 0.22 |
| Hypertension | 221 (72.0%) | 140 (79.5%) | 84 (75.7%) | 0.18 |
| Myocardial infarction | 149 (48.5%) | 87 (49.4%) | 65 (58.6%) | 0.18 |
| Heart failure | 51 (16.6%) | 35 (19.9%) | 27 (24.3%) | 0.20 |
| Stroke | 42 (13.7%) | 31 (17.6%) | 25 (22.5%) | 0.09 |
| Diabetes | 74 (24.1%) | 62 (35.2%) | 37 (33.3%) | 0.02 |
| Revascularization | 99 (32.2%) | 54 (30.7%) | 53 (47.7%) | 0.005 |
| Peripheral vascular disease | 20 (6.5%) | 12 (6.8%) | 13 (11.7%) | 0.21 |
| Smoking | 46 (15.0%) | 22 (12.5%) | 10 (9.0%) | 0.27 |
| Systolic blood pressure (mm Hg) | 135.9 ± 20.4 | 135.1 ± 17.9 | 135.9 ± 20.3 | 0.90 |
| Diastolic blood pressure (mm Hg) | 76.1 ± 10.5 | 73.9 ± 10.4 | 73.1 ± 10.4 | 0.01 |
| Body mass index (kg/m 2 ) | 28.6 ± 5.3 | 28.4 ± 5.1 | 28.4 ± 5.2 | 0.93 |
| Total cholesterol (mg/dL) | 165.0 ± 38.0 | 163.8 ± 42.9 | 160.5 ± 35.8 | 0.57 |
| HDL cholesterol (mg/dL) | 47.0 ± 15.7 | 46.8 ± 15.5 | 46.1 ± 13.5 | 0.85 |
| LDL cholesterol (mg/dL) | 93.6 ± 31.4 | 94.0 ± 35.4 | 93.1 ± 31.3 | 0.97 |
| Triglycerides (mg/dL) | 98 (67, 151) | 97 (68, 144) | 90 (64, 123) | 0.19 |
| Estimated glomerular filtration rate (mL/min) | 76.2 ± 23.6 | 73.2 ± 20.2 | 69.1 ± 19.2 | 0.01 |
| Calcium (mg/dL) | 9.5 ± 0.4 | 9.5 ± 0.4 | 9.5 ± 0.4 | 0.73 |
| Phosphorus (mg/dL) | 3.3 ± 0.6 | 3.3 ± 0.5 | 3.4 ± 0.5 | 0.005 |
| C-reactive protein (mg/dL) | 1.3 (0.7, 3.2) | 1.5 (0.7, 3.4) | 1.6 (0.7, 4.2) | 0.14 |
Study participants were followed for a median duration of 4.2 years (interquartile range 3.3 to 5.0 years). A total of 205 CV events were recorded, which included 152 deaths, 28 myocardial infarctions, 22 strokes or transient ischemic attacks, and 40 hospitalizations for heart failure. Participants with a composite calcium score of 0 had a significantly lower incidence of CV events than participants with a composite calcium score of ≥2 (5.5 vs 11.1 events per 100 person-years, p <0.001, Figure 2 ). Participants with a composite score of 0 also had significantly lower rates of death (3.6 vs 8.9 deaths per 100 person-years, p <0.001) and myocardial infarction (0.6 vs 2.1 events per 100 person-years, p = 0.01) compared with participants with a composite score of ≥2. The incidence of stroke or transient ischemic attack and hospitalization for heart failure did not differ significantly between the groups ( Figure 3 ).




