Upper-extremity Arteriovenous Hemodialysis Access
Michael J. Englesbe
Darrell A. Campbell Jr.
The National Kidney Foundation Dialysis Outcomes Quality Initiative Clinical Practice Guidelines for Vascular Access (DOQI) provide specific practice recommendations to the vascular access surgeon. These guidelines emphasize the benefits of autogenous arteriovenous accesses. Unfortunately, many of the complicated patients who present for hemodialysis access do not have superficial veins suitable for a primary autogenous access. We will discuss the pre-operative evaluation of these complex patients, a strategy for selecting the optimal access procedure, and our surgical technique. The clinical approach in this chapter is in concert with the DOQI guidelines.
Pre-operative Assessment
The evaluation of a patient for hemodialysis access begins with a complete history and physical examination. Specific attention should be paid to a history of previous access surgeries or dialysis catheters. Multiple failed attempts at access of unclear etiology should prompt a hypercoagulable evaluation. A frank discussion with the patient concerning the morbidity of access surgery will enable the patient to decide the hand in which to place the access (the nondominant hand is usually preferred).
The physical exam focuses on motor and sensory function of the upper extremities. The extremities are evaluated for edema and arterial inflow (bilateral upper-extremity blood pressures and pulse examination); an Allen test should be done. A difference in systolic blood pressure (SBP) of 15 mmHg or greater prompts a more complete evaluation of extremity arterial inflow (arterial duplex and possible angiogram).
Careful physical examination of the veins of the arm can be aided with a sphygmomanometer inflated on the upper arm to a pressure below systolic blood pressure to facilitate venous engorgement. A cephalic vein appropriate for use should be distensible, nonsclerotic, and at least 3 mm in diameter. The forearm basilic vein and occasionally the arm basilic vein should also be examined. If a usable segment of vein is found, then a pre-operative venogram or venous duplex can be avoided in patients who have not had previous long-term access catheters. Many patients will have adequate cephalic or basilic veins deeper in their arm, and an imaging study is appropriate to find 3 mm or larger veins that are amenable to transposition into the subcutaneous tissues or for prosthetic graft outflow.
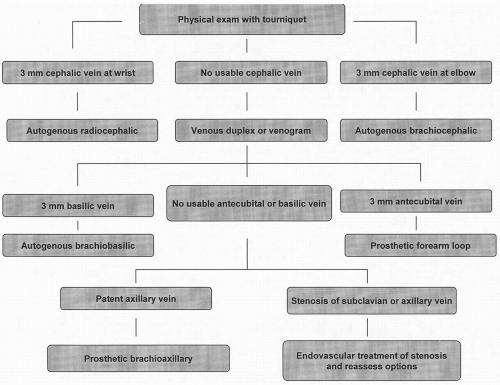
Access failure is usually related to venous outflow; thus a careful evaluation of the upper-extremity veins is indicated. Most of the clinical decisions hinge upon the quality of the cephalic, basilic, and axillary veins. Our basic decision tree for access in the standard patient is shown in Figure 84-1. Even though there are no randomized, controlled trials comparing autogenous to prosthetic upper-extremity accesses, autogenous accesses are preferred in most cases. The DOQI guidelines state that autogenous accesses should be constructed in at least 50% of all new kidney failure patients electing to receive hemodialysis as their initial form of renal replacement therapy. Our first choice for access is a radiocephalic autogenous access, and our second choice is the brachiocephalic autogenous access. Unfortunately, we estimate that only 20% of the patients who present for permanent hemodialysis access are candidates for one of these autogenous choices. Most of the patients who present have many risk factors for an inadequate cephalic vein that include extensive past medical histories, age greater that 65, and multiple previous peripheral intravenous catheters. These patients require imaging of the venous anatomy of their arm for adequate operative planning. We generally obtain a contrast venogram, but there are many studies indicating that venous duplex is an acceptable alternative. The imaging study may reveal both 3 mm or larger basilic and antecubital veins. These patients are candidates for either an autogenous brachiobasilic transposition or a prosthetic forearm loop.
There are no specific data to suggest that a strategy of performing autogenous brachiobasilic access prior to attempting a prosthetic forearm loop is the optimal strategy in patients with an inadequate cephalic vein. There is significant momentum to maximize autogenous access options, but transposition of the basilic vein is a significantly larger and more morbid procedure than a prosthetic forearm loop. When the prosthetic forearm loops fails, it is usually still possible to perform a brachiobasilic transposition. Furthermore, the prosthetic forearm loop may cause the basilic vein to further dilate and, therefore, be more amenable to a subsequent access. In our initial experience with autogenous brachiobasilic access, the primary and secondary patency rates were 47% and 64% at 1 year and 41% and 58% at 2 years, respectively (N = 99). Additionally, 23% of the accesses were never suitable for cannulation (primary failure). Although these outcomes are likely acceptable, they have likely improved as we have gained additional
experience. We are currently performing a randomized, controlled trial comparing the autogenous brachiobasilic and forearm prosthetic loop accesses.
experience. We are currently performing a randomized, controlled trial comparing the autogenous brachiobasilic and forearm prosthetic loop accesses.
Patients who do not have a suitable basilic or antecubital vein require a prosthetic brachioaxillary access. This usually is the final access option in the ipsilateral arm. A history of central venous catheters places a patient at risk for a venous (i.e., axillary, subclavian, brachiocephalic, or superior vena cava) outflow obstruction. Placement of an arteriovenous access in patients with significant central vein stenosis may lead to severe venous hypertension and access failure. If the central veins are stenotic or obstructed, the contralateral arm should be used, provided that there are suitable options. Alternatively, the central venous stenosis can be corrected with balloon angioplasty alone or in combination with intraluminal stenting.
Operative Technique
Autogenous Access
The autogenous radiocephalic access is the best option for patients with an acceptable cephalic vein at the wrist and normal radial artery inflow (Figs. 84-2A and 84-2B). This procedure can be done under local anesthesia or a regional block. A 3 cm longitudinal incision is made between the cephalic vein and the radial artery just proximal to the skin crease at the wrist. Alternatively, an incision can be made in the anatomic snuffbox. Approximately 2 to 3 cm of cephalic vein is dissected free from subcutaneous tissues, and the venous collaterals are ligated. We give all access patients intravenous heparin or we regionally heparinize the vessels prior to occluding the artery. The anastomosis can be done using four different configurations (end vein-side artery, side vein-side artery, end vein-end artery, side vein-end artery). We prefer the end vein-side of artery configuration using a 6 to 8 mm arteriotomy. This results in the highest flow through the fistula and is associated with a low risk of venous hypertension in the hand. Following construction of the anastomosis, a thrill should be palpable along the proximal course of the vein. A transmitted pulse without a thrill indicates an obstruction in the proximal vein. The vein can be probed with vascular dilators in an attempt to dilate the stenosis. An intraoperative venogram may determine the location of the stenosis, and venoplasty should be considered. If these techniques fail to produce a satisfactory thrill, the anastomosis can be resited more proximal on the radial artery or another access configuration should be constructed.
The autogenous brachiocephalic access is the second choice if the radiocephalic access is not an option (Figs. 84-3A and 84-3B). This procedure can also be done under local or regional anesthesia. We generally make an incision just below the elbow crease and construct the anastomosis in an end of vein-side of artery configuration. The vein needs to be dissected 5 to 7 cm along its length to avoid kinking as it courses from lateral to medial. The anastomosis should be no larger than 8 mm in an attempt to reduce the incidence of the ischemic complications that have been reported in up to 10% of cases after brachial artery-based procedures. We have not had much success with the autogenous brachiocephalic access in obese patients, although it is possible to elevate the cephalic vein more superficial in this setting. This can be performed at the time of the initial procedure, although it may be optimal to defer the elevation until the access dilates sufficiently for cannulation. The perforating branch of the median cubital vein can also be used as an alternative to the more traditional cephalic vein. This branch connects the superficial and deep venous systems of the arm. A segment of the deep vein can be dissected free and anastomosed to the brachial artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree