Unilateral Opaque Hemithorax
Dharshan Vummidi, MD
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Pleural Effusion
Empyema
Hemothorax
Pneumonectomy
Community Acquired Pneumonia
Less Common
Endobronchial Tumor
Non-Small Cell Lung Cancer
Small Cell Lung Cancer
Pleural Metastasis
Rare but Important
Pulmonary Agenesis
Fibrous Tumor of Pleura
Malignant Mesothelioma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Chest wall
CT and MR usually definitive
Absent mediastinal shift
Associated osseous lesions (e.g., fracture with chest wall hematoma)
Pleural
Obtuse margins with pleural interfaces
Contralateral mediastinal shift
CT and MR usually definitive
Pulmonary
Acute margins with pleural surface
Mediastinal shift varies depending on etiology
CT usually definitive
Helpful Clues for Common Diagnoses
Pleural Effusion
Contralateral mediastinal shift
Atelectasis of underlying lung
Meniscus sign: Lateral concave border where effusion meets costal pleura
Downward displacement of hemidiaphragm on left
Empyema
Lenticular shape
Nondependent location with clear demarcation from adjacent lung
Split pleura sign
Pleural fluid separates enhancing visceral and parietal pleura
Not specific for empyema: Occurs with any form of pleural inflammation
Haziness in adjacent extrapleural fat
Compresses adjacent lung and vessels
Presence of gas in absence of thoracentesis
Contralateral mediastinal shift
Hemothorax
High-attenuation pleural fluid (> 50 HU)
Usually unilateral
Blunt or penetrating trauma
Iatrogenic
Spontaneous causes include rupture of aneurysms, coagulopathy, pleural metastases, and pleural endometriosis
Pneumonectomy
Pneumonectomy space fills with fluid within 30 days
Ipsilateral mediastinal shift
New or increased gas in existing pneumonectomy space indicates bronchopleural fistula
Community Acquired Pneumonia
Lobar consolidation
S. pneumoniae most common
TB, H. influenzae, Legionella less common
Parapneumonic effusion
Can develop into empyema
Helpful Clues for Less Common Diagnoses
Endobronchial Tumor
Whole lung collapse less common than lobar collapse
Primary lung carcinoma: Squamous cell carcinoma most common
Metastasis: Breast, colon, and renal cell carcinoma; melanoma
Ipsilateral mediastinal shift
Non-Small Cell Lung Cancer
Extrinsic compression of main bronchus
Primary tumor, lymph node metastases, or both
Small Cell Lung Cancer
Extrinsic compression of main bronchus
Bulky lymph node metastases common
May also invade mediastinum
Pleural Metastasis
∽ 90% of all pleural neoplasms
Lung carcinoma leading cause
Breast, ovary, and gastric carcinomas and lymphoma also common causes
Usually multiple
Can simulate benign pleural disease
Nodular, circumferential, and mediastinal pleural involvement suggestive of malignancy
Associated pleural effusion common
Can have lung or thoracic lymph node metastases
Helpful Clues for Rare Diagnoses
Pulmonary Agenesis
Complete absence of lung with no bronchial or vascular tissue
Often associated with other congential anomalies, resulting in neonatal death
Adults with isolated pulmonary hypoplasia often asymptomatic
Identical imaging appearance to patients with childhood pneumonectomy
Fibrous Tumor of Pleura
5-10% of primary pleural neoplasms, 12% malignant
Imaging alone cannot determine whether malignant or not
Peak incidence: 6th and 7th decades
Approximately 50% patients symptomatic
Clubbing (4%)
Symptomatic hypoglycemia (4-5%)
Radiography
Solitary peripheral pleural mass with smooth margins
May develop within pulmonary fissure
Can change orientation with changes in patient position
CT
Smaller tumors homogeneous
Larger tumors heterogeneous with necrosis, cystic degeneration, and hemorrhage
Calcification (7-25%) (more common in larger tumors)
Has smooth margins, abuts pleural surface, and may form obtuse angles with adjacent pleura
Intense, uniform enhancement except in areas of necrosis
MR
Fibrous tissue: Low to intermediate signal intensity on T1- and T2-weighted imaging
Cystic degeneration, necrosis, myxoid: Foci of high T2 signal intensity
Low signal septa on T2-weighted imaging
Blood products: T1 and T2 signal intensity vary depending on age of hemorrhage
Malignant Mesothelioma
Most result from asbestos exposure
Latency of up to 40 years
Can simulate benign pleural disease
Nodular, circumferential, and mediastinal pleural involvement suggestive of malignancy
Mediastinum relatively “fixed” with little or no shift
Associated pleural effusion may be present
Extrapleural spread
Chest wall, mediastinum, diaphragm
Image Gallery
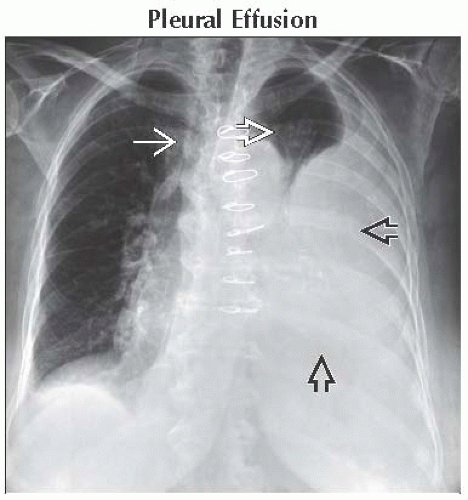 Frontal radiograph shows a large left pleural effusion
 causing marked left lung atelectasis with aeration of a small portion of the left upper lobe causing marked left lung atelectasis with aeration of a small portion of the left upper lobe  . Note rightward mediastinal shift . Note rightward mediastinal shift  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|