Unilateral Pleural Effusion
Toms Franquet, MD, PhD
DIFFERENTIAL DIAGNOSIS
Common
Parapneumonic Effusion
Neoplastic Diseases
Mesothelioma
Primary Lung Cancer
Breast Cancer
Pleural Metastases
Lymphoma
Hepatic Cirrhosis
Pancreatitis
Trauma
Less Common
Pulmonary Embolism
Myxedema
Rheumatoid Pleuritis
Chylothorax
Renal Disease
HIV Infection
Rare but Important
Catamenial Hemothorax
Yellow Nail Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Pleural effusions result from pleural, parenchymal, or extrapulmonary disease
Transudative effusions: Imbalance of hydrostatic and oncotic forces
Exudative effusions: From pleural diseases or decreased lymphatic drainage
CT generally more sensitive than radiography for detection of relatively small volumes of pleural fluid
Pleural pseudotumor: Accumulation of pleural fluid within interlobar fissure; vanishing tumors: Disappearance of effusions after treatment
Fluid in fissure has curvilinear edge concave to hilum
Minor fissure pseudotumor may be mistaken for pulmonary mass
Large and massive pleural effusions are more likely to be malignant
Half of malignant effusions do not reveal any pleural finding apart from effusion
Pleural nodules and circumferential pleural thickening are highly specific for malignancy
Ultrasonography: Useful to demonstrate pleural loculations
Fibrinous septations are better visualized on ultrasound than on CT scans
Helpful Clues for Common Diagnoses
Parapneumonic Effusion
Bacteria
In CAP, most commonly associated organisms are gram-positive aerobic bacteria
In nosocomial infections, gram-negative aerobes (H. influenzae, E. coli, P. aeruginosa, and Klebsiella)
CECT: Pleural thickening and loculated fluid; split pleura sign of empyema: Fluid between enhancing thickened pleural layers
Tuberculosis
Thick pleural rind: Usually unilateral
Fungi
Rare causes of pleural effusion
Neoplastic Diseases
Mesothelioma
Pleural thickening (89%)
Unilateral pleural effusion (87%)
Mediastinal pleural thickening (85%)
Primary Lung Cancer
Almost always ipsilateral pleural effusions
Infrequently bilateral
Breast Cancer
Ipsilateral pleural effusion in 83% of cases
Pleural Metastases
Adenocarcinoma most common tumor to metastasize to pleura
Thymomas may result in pleural dissemination: “Drop metastases”
CT: Irregular pleural thickening and small nodules at interlobar fissures
CECT: Variable enhancement
Lymphoma
Prevalence of pleural disease in both Hodgkin and non-Hodgkin lymphoma is similar (26-31%)
Usually occurs as part of disseminated disease
Contrast enhancement of parietal pleura
Coexistent involvement of parietal pleura, paraspinal region, and extrapleural space
Hepatic Cirrhosis
Associated with transdiaphragmatic movement of ascites
Right-sided, unilateral 70%; left sided 15%; bilateral 15%
Small to massive
Pancreatitis
Usually left-sided (70%) or bilateral (15%)
> pleural fluid amylase level is not specific indicator of pancreatitis
Pleural amylase values may be elevated in
Acute pancreatitis, pancreatic pseudocyst, rupture of esophagus, and ruptured ectopic pregnancy
Approximately 10% of malignant effusions have raised pleural amylase levels (especially adenocarcinoma)
Trauma
CT of acute hemothorax: Fluid-fluid level or increased density of pleural fluid
Helpful Clues for Less Common Diagnoses
Pulmonary Embolism
Pleural effusions in 30-50% of patients
Unilateral and small (85%)
Pleuritic pain: 75% of patients with pleural effusion
No specific pleural fluid characteristics
Pleural fluid red blood cell count > 100,000/mm3 suggests malignancy, pulmonary infarction, or trauma
Myxedema
Massive cardiomegaly (pericardial effusion) and thoracic inlet mass (goiter)
Unilateral or bilateral pleural effusions; small to moderate in size
Rheumatoid Pleuritis
Middle-aged men with positive rheumatoid factor
Chylothorax
Presence of chyle in pleural space: Malignancy (lymphoma and metastases), trauma, post-surgery, tuberculosis, LAM, sarcoidosis, and amyloidosis
Renal Disease
Peritoneal or hemodialysis
Like ascites-related pleural effusions, usually on right
HIV Infection
Causes of effusions: Kaposi sarcoma (30%), parapneumonic effusion (28%), tuberculosis (14%), Pneumocystis jiroveci pneumonia, and lymphoma
Helpful Clues for Rare Diagnoses
Catamenial Hemothorax
Occurs in 14% of patients with pleural endometriosis
85-90% occur on right (only 5% occur bilaterally)
Yellow Nail Syndrome
Rhinosinusitis, pleural effusions, bronchiectasis, lymphedema, and yellow nails
Image Gallery
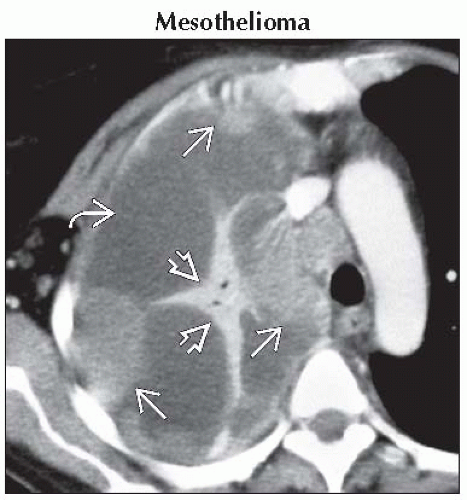 Axial CECT shows lobulated pleural thickening
 , loculated pleural effusion , loculated pleural effusion  , and compressed right upper lobe collapse , and compressed right upper lobe collapse  from malignant mesothelioma in the right hemithorax. from malignant mesothelioma in the right hemithorax.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|