Unilateral Mediastinal Mass
Toms Franquet, MD, PhD
DIFFERENTIAL DIAGNOSIS
Common
Thyroid Goiter
Thymoma
Teratoma
Lymphoma
Pericardial Cyst
Bronchogenic Cyst
Neurogenic Tumors
Pleuropericardial Fat Pad
Aortic Aneurysm
Less Common
Thymic Carcinoma
Thymic Cyst
Lymphangioma
Malignant Germ Cell Tumors
Esophageal Duplication Cyst
Rare but Important
Parathyroid Adenoma
Thymolipoma
Hemangioma
Meningocele
Thoracic Duct Cyst
Gastroenteric (Neurenteric) Cyst
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Chest radiograph is of limited value in differential diagnosis of mediastinal masses
Combination of location of mass, demographics, and imaging (CT, MR) may allow confident diagnosis
Clinical history is key in diagnosing lymphoma, extramedullary hematopoiesis, thymoma (myasthenia gravis), thymic carcinoid (hormone syndrome, e.g., Cushing or MEN)
Helpful Clues for Common Diagnoses
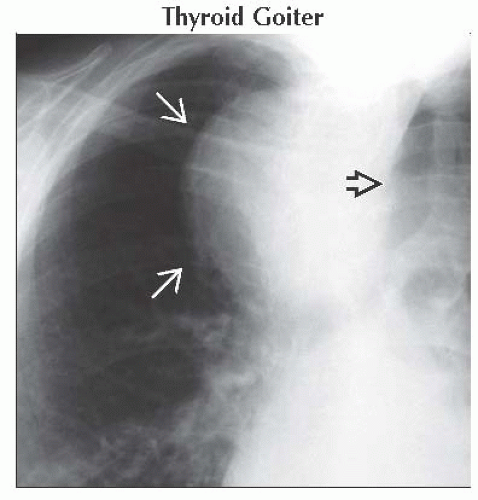
Thyroid Goiter
Most commonly in women
Right-sided mediastinal mass with contralateral tracheal displacement
High attenuation value (> 100 HU) on NECT
Thymoma
Well-defined, round or ovoid, anterior mediastinal mass
Variable size
Homogeneous or heterogeneous
Areas of hemorrhage, necrosis, or cyst formation (CT, MR)
Punctate, linear, or ring-like calcification (CT)
May result in pleural dissemination (“drop metastases”)
Teratoma
In anterior mediastinum (> 80%)
Adipose tissue component is common (> 80%)
Heterogeneous appearance on CT and MR
CT and MR useful to identify small foci of fat
Lymphoma
Non-Hodgkin lymphoma
Most frequent lymphoma (> 75%)
Large B-cell lymphoma: Young adults (20s and 30s), female predominance
Hodgkin lymphoma (nodular sclerosis)
Bulky anterior mass (40%)
Young adults (20s and 30s)
Pericardial Cyst
Usually in cardiophrenic angle
Bronchogenic Cyst
Variable origin: Paratracheal, carinal, hilar, paraesophageal, and extramediastinal
CT: 50% have high attenuation value (> 130 HU); wall calcification in 10%; rarely, milk of calcium in cyst fluid
Neurogenic Tumors
Neurofibroma
Paravertebral region or along nerve
Low attenuation value (20-25 HU) on NECT
Neurilemoma (schwannoma)
Paravertebral region or along nerve
Adjacent bone changes may be present (50%)
Ganglioneuroma
Predominantly in infants and children; 60% in patients < 20 years old
Low attenuation value on NECT
Ganglioneuroblastoma
Rare after age 10; oval lesions oriented in vertical axis (sympathetic chain)
Variable appearance: Homogeneous solid to cystic masses
Paraganglioma
Near base of heart and great vessels (adjacent to pericardium)
Usually bilateral; may be asymmetrical
Aortic Aneurysm
Consider aneurysm of any mass contiguous with any part of aorta
Helpful Clues for Less Common Diagnoses
Thymic Carcinoma
Most common histologic subtypes: Squamous cell carcinoma and neuroendocrine carcinoma
CT and MR: Irregular contour, necrotic or cystic component, heterogeneous contrast enhancement, great vessel invasion
Higher maximal standardized uptake values and homogeneous FDG uptake than thymoma
Thymic Cyst
Congenital
Unilocular; homogeneous water density (0-20 HU) on NECT
Wall imperceptible on CT
Acquired
Multilocular; higher attenuation than water
Evident cyst wall on CT
Lymphangioma
Usually found in neck or axilla; anterior mediastinum (10%); unilocular or multilocular (30%)
May insinuate around normal structures
Esophageal Duplication Cyst
Sharply marginated masses in middle or posterior mediastinum
CT: Round or tubular water attenuation masses near or within (intramural) esophageal wall
Helpful Clues for Rare Diagnoses
Parathyroid Adenoma
Most are very small; appearance similar to that of a lymph node
Optimal assessment by Tc-99m sestamibi combined with SPECT
Thymolipoma
Entirely asymptomatic
May mimic cardiomegaly
Positional changes in shape (soft consistency)
Hemangioma
Most are asymptomatic
Phleboliths visible (10%)
Heterogeneous appearance in both NECT and CECT
Meningocele
Classic location: Between thoracic inlet and diaphragm
Continuity between CSF in thecal sac and meningocele typical
Thoracic Duct Cyst
Small round or oval cystic mass in posterior mediastinum
Gastroenteric (Neurenteric) Cyst
Diagnosis: Childhood
Round or lobulated mass; homogeneously dense
Neurenteric: When it is associated with spinal column anomalies (symptomatic)
Image Gallery
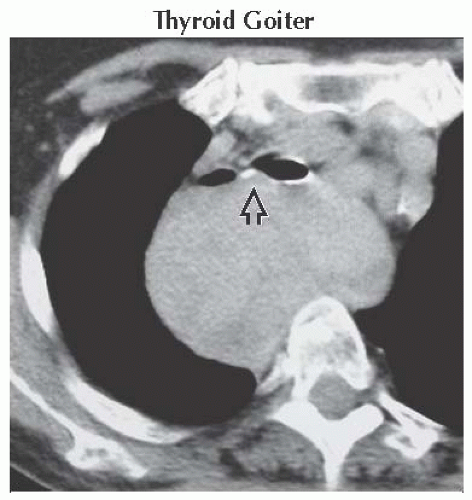 Axial NECT shows a large, homogeneous, middle mediastinal mass displacing the bronchi anteriorly with resulting airway compression
 . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|