Fig. 5.1
Panel (a) curvilinear ultrasound probe with a frequency range of 2–5 MHz. Panel (b) thoracic ultrasound performed pre-thoracoscopy with the patient in the lateral decubitus position

Fig. 5.2
Sterile sheath for ultrasound probe
5.3 Procedure at Thoracoscopy
Positioning of the patient differs from that preferred in the usual thoracic ultrasound assessment where patients are sat upright with their arms outstretched anteriorly. In thoracoscopy, the patient must be in the planned position for the port entry. Usually, this is the lateral decubitus position since this is the preferred position for medical thoracoscopy (and other pleural procedures under direct ultrasound guidance). Once the patient is correctly positioned, the transducer is held like a pen between the thumb and first fingers, with the medial aspect of the palm resting against the chest wall to enable the sonographer to remain steady and have a tactile awareness of their position whilst adjusting the images on the ultrasound machine to optimise their quality. The probe position should be orientated with the marker pointing towards the patients head, as is standard in sonography.
To ensure accurate orientation, a systematic approach is necessary where solid organs below the diaphragm should be identified first. Having identified the kidney, the probe is moved cranially to visualise the liver or spleen. Next, the costophrenic angle should be identified. The diaphragm should be examined by asking the patient to take deep breaths or sniff to ascertain the presence of paradoxical movement or any unexpected significant lung/organ excursions. Following this, the presence of pleural fluid is assessed. The ultrasonographic features of the space should be recorded, including the dimensions and characteristics of the pleural fluid. The position for trocar placement is then identified, and that location is further interrogated by tilting the transducer caudally and cranially to ascertain a three-dimensional representation of the area. This helps to ensure the absence of tethered viscera, septations, significant lung excursion on inspiration and interposition of subdiaphragmatic organs. Furthermore, this entry position should preferably still remain within the classical safe triangle (Laws et al. 2003). The site should be marked and the patient must maintain their position. If any adjustment is made, the site should be reassessed. By performing thoracic ultrasound using sterile conditions at the start of the procedure, the time between confirming position and port entry is minimised and in our opinion is the safest method.
5.4 Ultrasound Features
5.4.1 General Appearance
In thoracic ultrasound of the normal thorax, sound waves do not penetrate the lung due to the interface between the soft tissue and lung (predominantly air) having a poor acoustic impedance match leading to most of the sound waves being reflected back to the transducer. However, information can be obtained by confirming the presence of a pleural stripe which represents the acoustic reflection from the solid parietal and visceral pleura. At the costophrenic angle, the subdiaphragmatic organ will be obscured by the lung during respiration, whilst the diaphragm will not be fully visualised due to obscuring by the normal lung (Fig. 5.3). The normal movement of the lung is inferred by the presence of the sliding lung sign, which actually represents the movement between the parietal and visceral pleural surfaces. The absence of this sign may indicate pleurodesis or a pneumothorax, the two being distinguished by the presence or absence of comet tails (distal reverberation echoes), respectively. If previous pleurodesis has been performed, absence of the lung sliding sign would suggest that the lung may not fully deflate upon trocar insertion. In such cases, an alternate diagnostic approach may be considered.
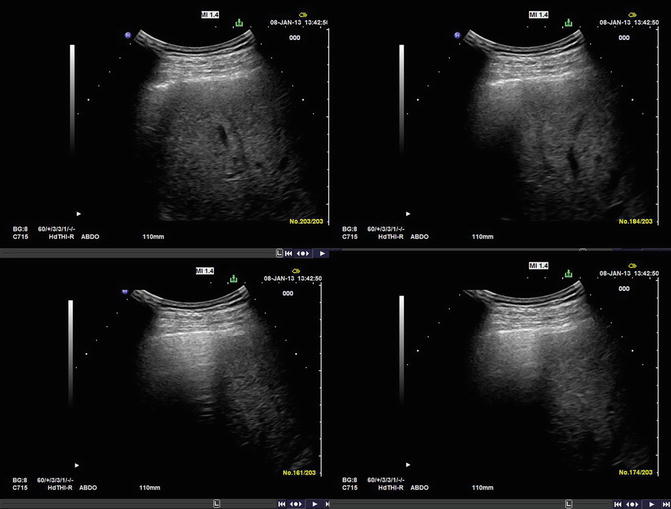
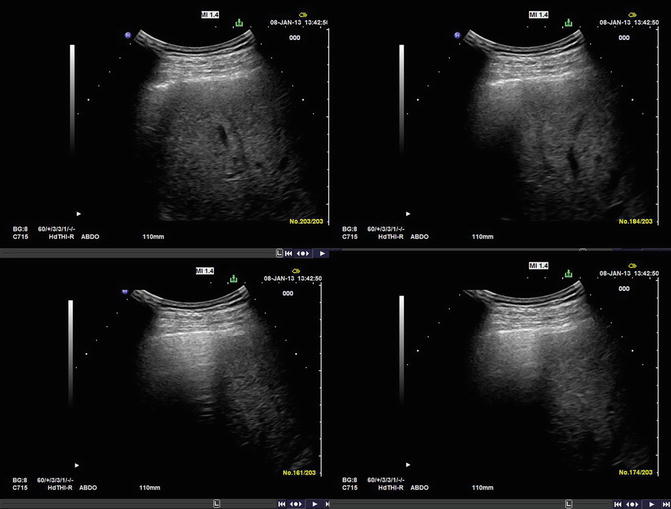
Fig. 5.3
Appearances of normal pleural cavity without fluid. The lung progressively obscures the liver during the respiratory cycle
5.4.2 Pathological Changes
Collections within the pleural cavity can be observed by the presence of echogenic regions bordered by the parietal pleura, diaphragm and underlying lung (Fig. 5.3). However, the ultrasonographic images are highly variable and therefore experience is required to interpret complex pleural spaces (Figs. 5.4, 5.5, and 5.6). Finally, the intercostal arteries have been shown to be variable in their position in relation to the superior rib, especially in the paravertebral region of the posterior ribs and in more elderly patients with ectatic vessels (Dewhurst et al. 2012; Yoneyama et al. 2010). Even within the safe triangle, Doppler signals may be utilised to identify aberrant vasculature underlying the area of port of entry.

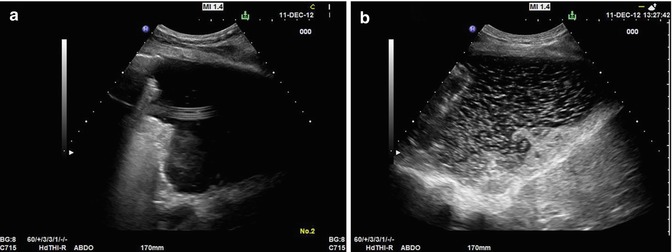

Fig. 5.4
A complex multiloculated pleural space secondary to malignancy
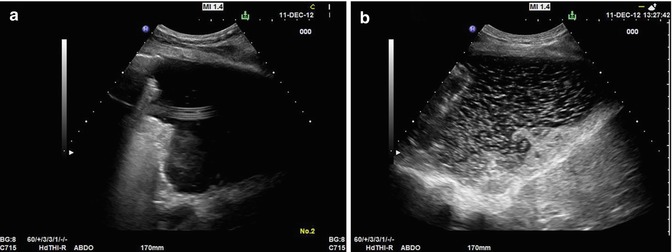
Fig. 5.5
A malignant pleural effusion secondary to oesophageal cancer (panel a). The space is highly echogenic and this is accentuated with patient movement (panel b). In addition, an indwelling pleural catheter can be seen crossing the space in panel (a)
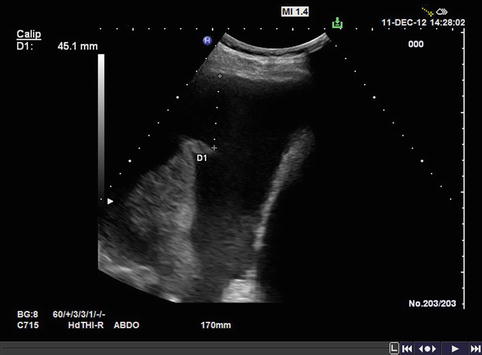
Fig. 5.6
A malignant pleural space secondary to lung cancer. There is evidence of swirling within the fluid. In addition, the underlying lung is atelectatic
Identifying abnormalities during assessment with thoracic ultrasound may lead the clinician to identify alternative diagnostic strategies. Quereshi et al. noted features of malignant and benign pleural effusions, showing a sensitivity of 79 % and specificity of 100 % (Qureshi et al. 2009). Features supporting malignant disease included parietal pleural thickening >1 cm, parietal pleural nodularity, visceral pleural thickening/nodularity and nodular or thickened diaphragms. Skilled assessment with the thoracic ultrasound may lead to alternative diagnostic pathways that are less invasive. Further, the poor ability to predict adhesions or septations and predict the complexity of the pleural space by CT scanning makes this a useful modality (Kearney et al. 2000).
Probably the most important role of thoracic ultrasound in medical thoracoscopy is to ensure successful entry into the pleural space (Hersh et al. 2003). Studies have demonstrated the role of ultrasound in identifying adhesions which could limit access to the pleural cavity and possibly result in procedural-related complications. Ultrasound has been shown to be superior to CT scanning in identifying pleural adhesions. Medford et al. demonstrated that ultrasound pre-thoracoscopy allowed for the identification of adhesions in all cases compared to a rate of detection of only 12.5 % by CT scanning in the non-ultrasound group (Medford et al. 2010). Further, in their study, there was no failure to access the pleural space in the ultrasound group compared to a failure rate of 16.7 % in the non-ultrasound group. Additional important features were revealed by ultrasound in 43 % of cases. Other authors have reported similar results. Cassanelli et al. in a surgical series reported that thoracic ultrasound had a sensitivity of 80.6 % (95 % confidence interval, 0.740–0.872) and specificity of 96.1 % (95 % confidence interval, 0.949–0.973) for the detection of adhesions – confirmed at VATS (Cassanelli et al. 2012). Wei et al. also demonstrated a sensitivity of 88 % and specificity of 82.6 % for the detection of adhesions and showed there to be good agreement between ultrasonographers (Wei et al. 2012).
5.4.3 Practical Considerations
Practical concerns over pre-thoracoscopy ultrasound may be the perceived lengthening of procedure time as a result of performing a scan. Macha et al. reported on a case series of 687 patients with pleural disease and found that ultrasound used prior to thoracoscopy saved the usual 20–30 min of time needed to induce a pneumothorax (Macha et al. 1993). This is supported by a further study suggesting that thoracic ultrasound adds only minutes to the length of the procedure (Hersh et al. 2003).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


