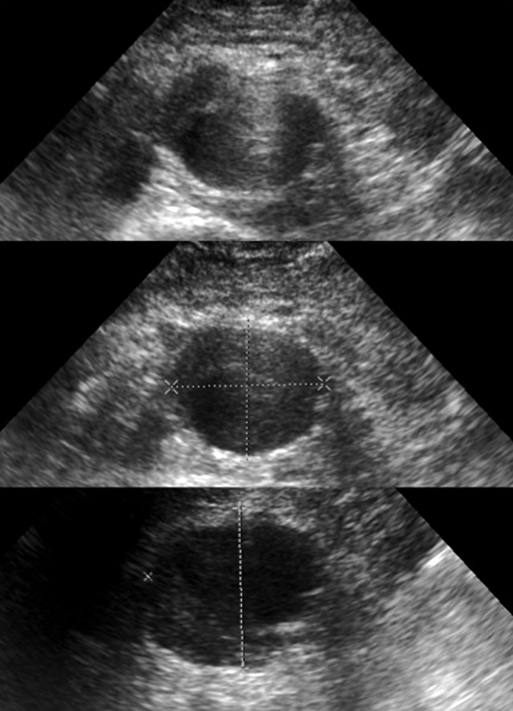
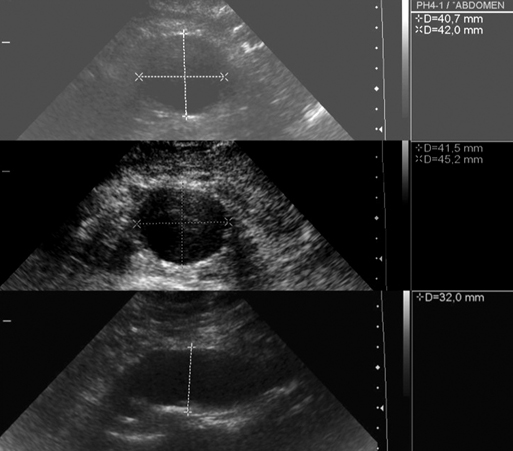
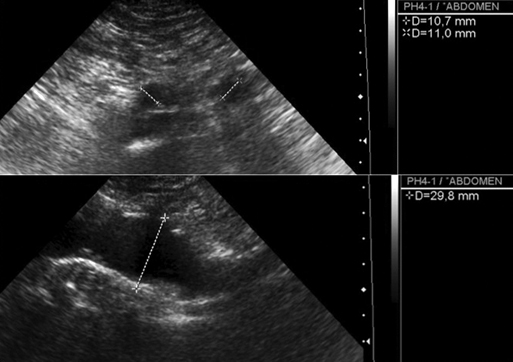
The maximum anteroposterior, transverse, and lateral aortic diameter measurements must be made from outside wall to outside wall perpendicular to the aortic axis, especially in tortuous aortas (Figure 1). Oblique measurements can overestimate the diameter. The origins of the celiac trunk, the superior mesenteric artery, and the renal arteries can all be individually documented. Careful evaluation of the course of the renal arteries and aorta in multiple planes can clarify the relation of the aneurysm to the renal arteries in case of juxtarenal AAA, although computed tomography (CT) scanning or aortography usually is required to evaluate this relationship precisely. Also, the transverse diameter of the remaining perfused lumen and the thickness and distribution (circumferential or eccentric) of intraluminal thrombus can be visualized and measured (Figure 2). Flow within the AAA may be laminar or turbulent. Turbulent flow is associated with the development of mural thrombus. The ultrasonographic appearance of a ruptured AAA is that of a large, usually hypoechoic retroperitoneal fluid collection surrounding the dilated aorta. Finally, the common iliac arteries can be imaged and measured in anteroposterior, transverse, and lateral planes (Figure 3). AAAs fulfill the World Health Organization (WHO) criteria for implementing a worthwhile screening program (Box 1). AAAs are common in men older than 65 years. They generally develop slowly and remain asymptomatic for years until reaching a stage involving danger of rupturing. An AAA can be diagnosed by ultrasonography inexpensively, noninvasively, and with high reliability, sensitivity, and specificity, whereas physical examination alone is often inaccurate. Ultrasound is currently the preferred method for AAA diagnosis. It is noninvasive, without known risks, readily available, straightforward to learn as a focused examination, accurate, and inexpensive. The sensitivity of ultrasound scanning for AAA is 95%, and the specificity approaches 100%. Portable ultrasound can further decrease the cost of screening up to 80% and is easier to use in outpatient and primary care settings, with a reported sensitivity of 93% and specificity of 97% for diagnosis of an AAA.
Ultrasonography in the Evaluation of Abdominal Aortic Aneurysms
Screening for Abdominal Aortic Aneurysm
Ultrasonography in the Evaluation of Abdominal Aortic Aneurysms