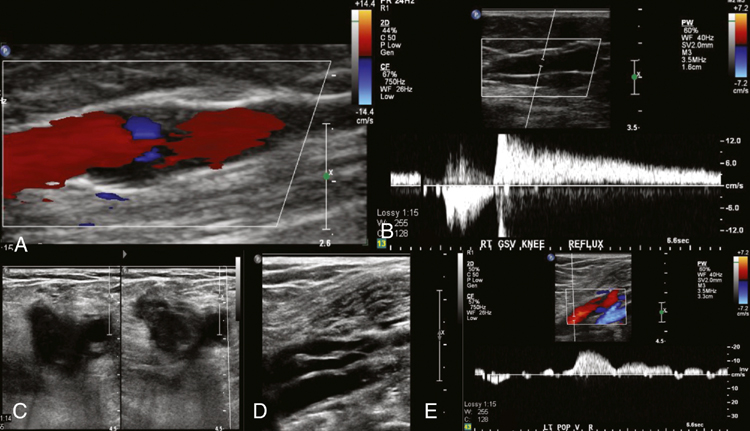
The advent of duplex ultrasound has allowed the assessment of the venous anatomy and function in real time (Figure 1). It has several advantages: It has low cost and it is portable, safe, easy to repeat, noninvasive, and the best method to identify reflux and obstruction at the same time. It is also used to guide treatment and assess the results. Complementary to venous duplex ultrasound are physiologic tests such as plethysmography, which may be indicated to gauge the severity of reflux or calf muscle pump function.
Ultrasonography for the Diagnosis of Venous Disease
Thoracic Key
Fastest Thoracic Insight Engine



