Type B2 Thymoma (Lymphoepithelial or Cortical Thymoma)
Borislav A. Alexiev, M.D.
Fabio R. Tavora, M.D., Ph.D.
Terminology
Type B2 thymoma is an organotypic thymic epithelial neoplasm composed of large, polygonal tumor cells that are arranged in a loose network and exhibit large vesicular nuclei with prominent large nucleoli, closely resembling the predominant epithelial cells of the normal thymic cortex.1 A background population of immature T cells is always present and usually outnumbers the neoplastic epithelial cells.2 The postulated cell of origin is a thymic epithelial cell capable of differentiating toward cortical-type epithelial cells.2
Incidence and Clinical
Type B2 thymoma accounts for ˜18% to 42% of all thymomas and depends on the study cited.3,4 Patients’ ages range from 13 to 79 years, with a mean of 47 to 50 years.3,4,5 There is no consistent gender predominance.6,7
The most frequent manifestations are symptoms of myasthenia gravis in 30% to 82% of cases.3,4,6,8,9 Rare complications are hypogammaglobulinemia (Good syndrome) and pure red cell anaplasia.10 Patients with type B2 thymoma may experience symptoms caused by compression of the surrounding organs by an expansive mass. These problems may take the form of superior vena cava syndrome, dysphagia, cough, or chest pain. Some patients with type B2 thymoma have no symptoms at all, and the tumor can be detected for an unrelated problem as an enlarged mediastinal area or mass by x-ray, CT, or MRI.
Gross Pathology
Grossly, type B2 thymomas are encapsulated or vaguely circumscribed.9 The cut surface is soft or firm and exhibits a tan nodular/lobular architecture. There may be cystic changes, hemorrhage, and fibrosis.2 The tumor can invade mediastinal fat or adjacent organs.
Microscopic Pathology
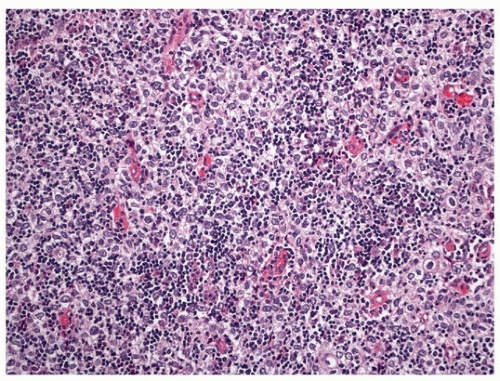
Histologically, B2 thymoma demonstrates a coarse lobular architecture with irregular septa (Fig. 101.1), somewhat resembling the lobular architecture of the normal thymic cortex. The neoplastic cell component consists of a prominent large polygonal epithelial cell population with vesicular nuclei and prominent nucleoli admixed with numerous lymphocytes (Figs. 101.1 and 101.2). The neoplastic epithelial cells form a delicate loose network, forming palisades around perivascular spaces and along septa. The tumor lacks extensive areas of virtually pure epithelial cells or pure lymphocytes. This type of thymoma resembles type B1 thymoma in its predominance of lymphocytes, but foci of medullary differentiation are less conspicuous or absent. Lymphocytes may outnumber the epithelial cells but do not obscure them. Lymphoid follicles in perivascular spaces or septa are more frequent in myasthenia gravis-associated cases.
Special Studies
The neoplastic cells strongly express a CK5/6, CK903, and p63 pattern similar to normal cortical thymocytes (Fig. 101.3). Focal positivity for CK8/18 and CK7 may also be observed.2 Epithelial membrane antigen (EMA), CK20, CD20, CD117, and CD5 stains are negative in tumor cells.11 Admixed intratumoral lymphocytes demonstrate a cortical immature T-cell immunoprofile: TdT+, CD1a+, CD99+, CD3+, CD4+, CD8+, and CD5+ with high proliferation rate (Figs. 101.4 and 101.5).12 Lymphocytes in rare medullary islands are mostly mature T cells: CD3+, CD5+, CD1a-, CD99-, TdT-, and significantly less proliferative.5,6,13,14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree