Type B1 Thymoma (Lymphocyte-Rich or Predominantly Cortical Thymoma)
Borislav A. Alexiev, M.D.
Fabio R. Tavora, M.D., Ph.D.
Terminology
Type B1 thymoma is an organotypic thymic epithelial neoplasm composed predominantly of areas resembling thymic cortex with epithelial cells scattered in a prominent population of immature lymphocytes, and areas of medullary differentiation, with or without Hassall corpuscles. The postulated cell of origin is a thymic epithelial cell capable of differentiating toward both cortical and medullary type.1
Incidence and Clinical
B1 thymoma is a relatively rare tumor of the adult age (mean of 41 to 47 years) with no significant difference in the distribution of genders. B1 thymoma accounts for 4% to 26% of all thymomas and is often diagnosed because of associated immunologic diseases such as myasthenia gravis (18% to 56% of the cases).2,3,4,5,6 Patients with type B1 thymoma may experience symptoms caused by compression of the surrounding organs by an expansive mass. Some patients with type B1 thymoma have no symptoms at all, and the tumor can be detected for an unrelated problem as an enlarged mediastinal area or mass by x-ray, CT, or MRI.
Gross Pathology
Grossly, B1 thymoma is usually a well-defined or encapsulated grayish mass. Thick fibrous capsule and septa can be present, as well as cystic spaces or small hemorrhagic and necrotic areas.
Microscopic Pathology
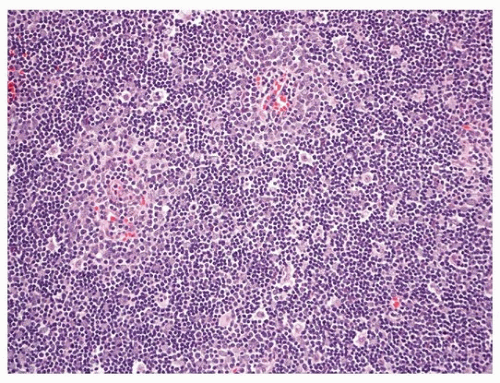
Histologically, B1 thymoma closely resembles normal thymic cortex with interspersed medullary foci.1,7 The tumors may grow in expansile sheets or display a highly organoid lobular architecture. Unlike the normal thymus, the lobules are of varying sizes and separated by thin or thick acellular fibrous septa. The neoplastic epithelial component is relatively inconspicuous and appears as interspersed oval cells with pale round nuclei and small nucleoli, although some cells may be large and occasionally have conspicuous nucleoli (Figs. 100.1 and 100.2). Long dendritic processes may be visible, best seen on keratin stains. The epithelial cells are dispersed and usually do not form cellular groupings. The lymphoid component is a densely packed population of small lymphocytes with clumped chromatin. Tangible-body macrophages may be scattered throughout giving rise to a starry-sky appearance. Perivascular spaces are not as frequent as in the other B thymomas. Cystic spaces and areas of necrosis, when present, are usually small. Pale areas of medullary differentiation are always present, composed of more loosely packed lymphocytes (Fig. 100.3). Hassall corpuscles may be seen but are less numerous than in normal medulla. They range from poorly formed epithelial groupings to large structures with prominent keratinized centers.
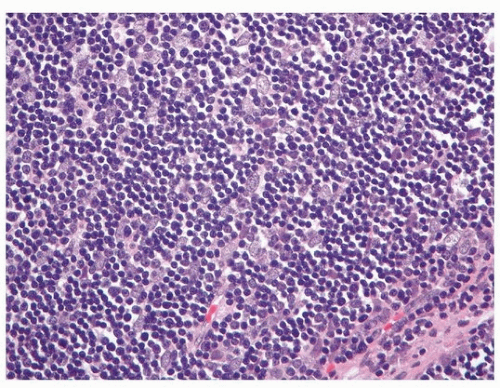 FIGURE 100.2 ▲ Type B1 thymoma. The neoplastic epithelial component is relatively inconspicuous and appears as interspersed oval cells with pale round nuclei and small nucleoli (H&E, ×400). |
Special Studies
The neoplastic cells strongly express a CK5/6 (Fig. 100.4), CK903, and p63 pattern similar to normal cortical thymocytes. Focal positivity for
CK8/18 and CK7 may also be observed. The proliferative index (Ki-67) is low.8,9 EMA, CK20, CD20, CD117, and CD5 stains are negative in tumor cells.10 Admixed lymphocytes demonstrate a cortical immature T-cell immunoprofile (TdT+, CD1a+, CD99+, CD3+, CD4+, CD8+, CD5+) (Fig. 100.5) with high proliferation (Ki 67) rate.10 In contrast, lymphocytes in the medullary islands are mostly mature T cells (TdT-, CD1a-, CD99-) and B cells (CD20+) (Fig. 100.6).10
CK8/18 and CK7 may also be observed. The proliferative index (Ki-67) is low.8,9 EMA, CK20, CD20, CD117, and CD5 stains are negative in tumor cells.10 Admixed lymphocytes demonstrate a cortical immature T-cell immunoprofile (TdT+, CD1a+, CD99+, CD3+, CD4+, CD8+, CD5+) (Fig. 100.5) with high proliferation (Ki 67) rate.10 In contrast, lymphocytes in the medullary islands are mostly mature T cells (TdT-, CD1a-, CD99-) and B cells (CD20+) (Fig. 100.6).10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree