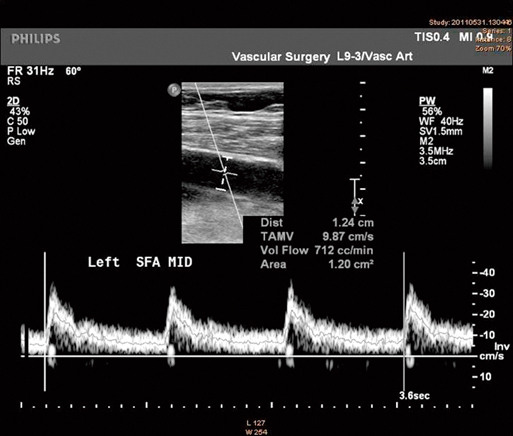
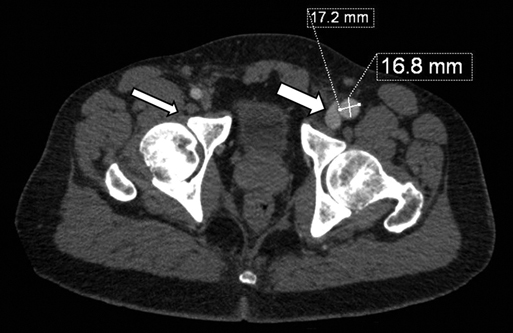
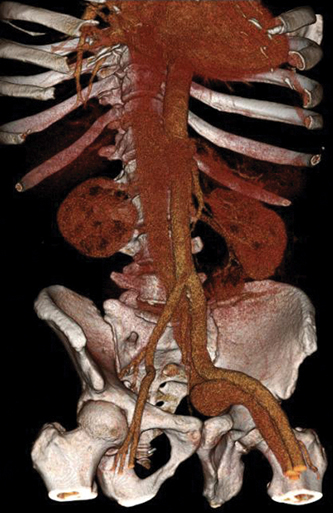
Suspicion for an AVF mandates imaging for confirmation. Duplex ultrasonography (US) is the initial imaging test of choice for the diagnosis of neck or extremity AVF. Doppler flow with color images can depict a direct connection between the artery and vein. The hallmarks of AVF on duplex include turbulent flow in the venous segment adjacent to the AVF, increased diastolic flow in a dilated artery proximal to the lesion, and decreased or retrograde arterial flow distal to the suspected site of the AVF (Figure 1). Anatomic constraints limit the accuracy of US in evaluating suspected AVF in the thoracic outlet, chest, abdomen, and pelvis. In these locations, CT angiography (CTA) is the diagnostic modality of choice in most centers. Hallmarks of an AVF on CTA include dilated veins and early venous filling (Figure 2). If the imaging during a CTA is timed appropriately, there should be opacification of arteries with contrast, but little or no venous opacification. Substantial venous opacification, especially when asymmetric, is a strong clue to the presence of an AVF (Figure 3). Engorged veins with large numbers of venous collaterals are additional CTA findings that suggest an AVF (Figure 4). The gold standard for the diagnosis of traumatic AVF is digital subtraction arteriography (DSA). The classic findings of an AVF are early venous filling at the site of the AVF with diminished distal arterial opacification (Figure 5). Small or branch vessel AVFs may be difficult to discern at first glance, and the actual arteriovenous connection might not be visualized in all cases. However, any early venous filling on arteriography should prompt selective catheterization to confirm the presence of an AVF and identify the parent artery and vein that give rise to the AVF. Other arterial abnormalities may also be identified, including an associated pseudoaneurysm or intimal flap. The sensitivity of arteriography to diagnose arterial injuries, including AVF, approaches 100% in experienced hands.
Treatment of Traumatic Arteriovenous Fistulas
Clinical Presentation and Diagnosis

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine

