Treatment of Recurrent Extracranial Carotid Occlusive Disease
Gregory A. Carlson
Timothy F. Kresowik
The term “recurrent carotid stenosis” generally includes the entire spectrum of patients who develop carotid disease after surgical or endovascular intervention. The frequency of carotid endarterectomy (CEA) has increased over the last decade largely because of the randomized trials, which established the efficacy of the procedure. The combination of increased carotid intervention and the availability of a noninvasive, relatively inexpensive method (duplex scanning) of follow up has resulted in increasing identification of patients with recurrent disease. The actual incidence of recurrent stenosis depends on the definition of recurrence, the techniques employed in the primary procedure, and the follow-up interval. In the Asymptomatic Carotid Atherosclerosis Study (ACAS), which included prospective duplex surveillance, there was a 12% incidence of residual or recurrent stenosis to the 60% or greater level at 5 years.
While the treatment of primary carotid stenosis has a relatively strong evidence base from multiple prospective, randomized trials, the evidence for treatment of recurrent lesions is largely based on retrospective reviews. It is not at all clear that a recurrent lesion carries the same risk of stroke without intervention as a primary lesion, and there is some evidence that the risk may be lower for recurrent lesions at similar degrees of stenosis. The decision to intervene requires detailed consideration of each individual patient. Redo CEA mandates a thorough understanding of cervical anatomy, as the risk of local complications such as cranial nerve injury is increased in the scarred dissection field. Overall, patients with recurrent carotid disease must be approached cautiously and deliberately, with a complete understanding of both the goals of therapy and the potential risks.
Diagnostic Considerations
Most recurrent lesions are identified by routine duplex surveillance. Less frequently, the diagnosis will be made by duplex evaluation for new neurologic symptoms. Extensive duplex evaluation is mandatory to plan for intervention. Much of the pertinent anatomy necessary to understand the type of pathologic lesion present and the optimal method of treatment can be gleaned from duplex evaluation.
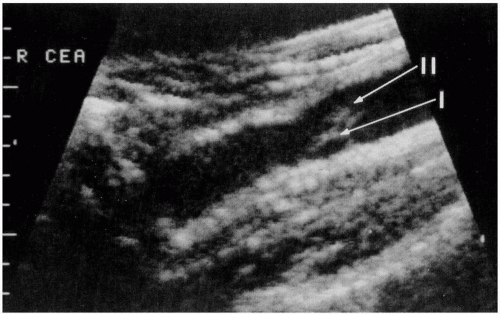
The duplex evaluation of recurrent carotid disease should include much more than percent stenosis. The lesion should be examined in B-mode ultrasound along its entire length; this evaluation can distinguish the long, smooth narrowing of myointimal hyperplasia from the irregular plaques of atherosclerotic disease. Understanding the etiology of the lesion may help predict the risk for a neurologic event and will clearly help to plan surgical or endovascular intervention. It has been suggested that the likelihood of symptoms might be predicted based on such factors as heterogeneity of the plaque on ultrasound examination. In addition, the location and length of the lesion can be assessed. Importantly, those recurrent lesions that occur in the native internal carotid distal to the previous endarterectomy endpoint can extend high up in the neck, and surgical exposure for redo CEA will be more challenging and risky in these patients.
While further imaging with intra-arterial digital subtraction angiography (IADSA), magnetic resonance angiography (MRA), or computed tomographic angiography (CTA) is not mandatory in patients with recurrent carotid stenosis, these patients are more likely to require these additional studies than those with primary stenosis. In patients who present with symptoms from recurrent disease, especially the myointimal hyperplasia type, attributing the neurologic event to the cervical carotid artery should be approached with some skepticism. While recurrent lesions can become symptomatic, it appears to be less common than in primary lesions, especially in hyperplastic lesions. Therefore, consideration should be given to evaluating the patient for other sources of emboli, such as the aortic arch and the intracranial circulation. Additionally, some of these lesions will extend higher in the neck than primary lesions, and duplex may not always be adequate to image the entire vessel in question. Finally, if endovascular intervention is being considered, these imaging studies can evaluate the aortic arch and proximal carotid artery for variants such as the bovine arch, which would make carotid artery stent (CAS) placement more challenging. Given the increased risks of secondary intervention and the poorly understood neurologic event risk in these patients, the surgeon should have a lower threshold for ordering these additional diagnostic tests to ensure that the lesion in question is completely understood prior to any intervention. The emergence of angiographic reconstructions with MRA and CTA has allowed us to avoid IVDSA and gain this valuable information with significantly less risk to the patient.
Pathogenesis
Generally, the etiology of the recurrent disease is categorized based on the length of time that has passed since the initial endarterectomy. These lesions can be separated into three categories. The first group of lesions (residual disease) occurs immediately following surgery, the second group (early recurrence) occurs during the first 2 years, and the third group (late recurrence) occurs greater than 2 years after intervention. These temporal guidelines are helpful in estimating the type of lesion involved; however, the disease process may be viewed as a continuum, and correlation with imaging studies is necessary. The pathogenesis of the lesion may be an important tool in determining optimal management of the recurrent carotid lesion.
The first group, those lesions presenting immediately following surgery, does not truly constitute a recurrent lesion. In some series with routine prospective follow up, residual stenosis accounts for as much as 1/3 of “recurrent” stenosis. These lesions are usually secondary to technical problems or thrombosis during or immediately following surgery, and they should be largely avoidable with careful operative technique. Residual, nonadherent shelves left at either endpoint can lead to a flap and stenosis once blood flow is restored (Fig. 30-1). Peri-operative antiplatelet therapy, including having adequate antiplatelet activity at the time of the procedure, is important in reducing the incidence of thrombus formation at the endarterectomy site, which can be a cause of not only peri-operative stroke but and also lead to residual/recurrent stenosis. The use of patch angioplasty rather than primary closure has been shown to both decrease the incidence of peri-operative events and also decrease the incidence of residual/recurrent stenosis. Finally, the repaired artery should be inspected following endarterectomy and closure. This can be accomplished by intraoperative duplex evaluation or completion angiography. Should any significant lesions be detected with these methods, the artery should be reopened, inspected, and repaired. With careful technique, residual stenosis is a largely avoidable occurrence.
The second group of stenoses (early recurrence) occurs in patients who present with a new stenosis up to 2 years following CEA. Following endarterectomy, the vessel wall undergoes a repair process, during which local myointimal cells proliferate and generate collagen and mucopolysaccharides along the traumatized segment of artery. In some patients, for reasons that are poorly understood, this process will be exaggerated, leading to a hyperplastic fibrous narrowing of the lumen of the carotid artery. This lesion is referred to as intimal or myointimal hyperplasia. Although the term “early recurrence” is used for lesions that appear within 2 years of CEA, the typical early recurrence due to myointimal hyperplasia is usually apparent by 6 months, and in many cases some abnormality is detectable within the first 3 months. Early recurrent stenoses may progress but are rarely associated with symptoms or occlusion within the first year. The typical lesion is very fibrous with a smooth surface, which is the likely reason for the apparently lower embolic potential.
Technical factors may be an issue for early recurrence. Minor defects with some flow disturbance but not meeting the level of a “residual stenosis” are associated with a higher likelihood of an early recurrent stenosis. Early recurrence is more common in women, and it has been attributed to the generally smaller vessels. Antiplatelet therapy does not appear to decrease the incidence of early recurrence. The only factor that has been clearly associated with a lower incidence of recurrent stenosis is the use of patch angioplasty rather than primary closure. Whether this is due to a better flow profile by widening the lumen at endpoints and thus avoiding flow disturbance, or to the fact that the overall lumen is widened and thus any intimal thickening is less likely to cause a narrowing, is not clear. The decreased incidence of recurrent stenosis associated with patching is most likely a combination of the two.
Those lesions presenting greater than 2 years after initial CEA (late recurrence) are most frequently attributed to progressive atherosclerotic disease. It must be realized that the distinction between early and late recurrence is somewhat blurred. The myointimal hyperplasia associated with early recurrence may be a precursor of the more advanced atherosclerotic plaque. These lesions can be varied in their location. In some cases, they will be in the native internal carotid artery just distal to the most cephalad extension of the endarterectomy plane. In other cases, atherosclerosis recurs directly in the treated lumen. The risk factors for progressive atherosclerosis mirror those that have been implicated in primary carotid artery disease. Namely, hypertension, hypercholesterolemia, and diabetes have all been implicated and should be aggressively controlled in these patients. In addition, cessation of cigarette smoking is essential to help avoid recurrent atherosclerosis. In addition to these risk factors, vascular wall injury during CEA may accelerate the atherosclerotic progression in some patients. Progressive disease occurring just distal to the endarterectomized site may be related to clamp placement. Care should be taken to minimize this risk by using atraumatic vascular clamps, applying the clamps only once, and avoiding vigorous manipulation of the vessel with the clamp in place.
Indications and Contraindications
The management of recurrent carotid stenosis remains controversial. Although some reports have suggested a higher stroke risk for redo CEA than primary procedures, there is evidence that, when adjusted for patient risk factors, the risk of peri-operative stroke and death is similar for primary and secondary CEA. There appears to be a higher risk of local complications, particularly cranial nerve injuries, associated with redo CEA. This makes sense because a scarred operative field presents more difficulty in identifying normal anatomy. The not uncommon need for a more distal dissection in redo CEA also increases the risk to cranial nerves that might not otherwise be in the usual dissection field. The decision to intervene and the type of intervention should be based on the balance between the risks of intervention and the risk of stroke with medical therapy alone.
For symptomatic recurrent carotid stenosis, it is generally accepted that intervention should be performed. As noted earlier, care should be taken to ensure that no other lesion is the cause of the neurologic event. The neurologic symptoms should correlate in type and distribution to the artery in question. Asymptomatic lesions, on the other hand, present more challenges for decision making. The natural history of these lesions is less predictable. It is clear that certain lesions will regress and actually become less stenotic over time, while other lesions will stabilize, and still others will progress to further stenosis and even occlusion. Technical problems noted immediately after the first endarterectomy should be almost universally repaired. Lesions noted after that point must be evaluated individually. Because myointimal lesions have been noted to regress, a somewhat conservative approach is warranted for early restenosis during the first year.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree