Treatment of Nonatherosclerotic Causes of Infrainguinal Arterial Occlusive Disease
Gregory J. Landry
Atherosclerosis is the most frequent cause of lower-extremity arterial occlusive disease. Most patients with atherosclerosis have wellknown risk factors, including advanced age, a history of smoking, diabetes mellitus, renal failure, hypertension, or hyperlipidemia. Occasionally, patients present with the typical symptoms of lower-extremity arterial occlusive disease, such as intermittent claudication, rest pain, or ischemic ulcerations, without the usual atherosclerotic risk profile. A variety of rare, but well recognized, nonatherosclerotic forms of lower-extremity occlusive disease have been described. Knowledge of the diagnosis and management of nonatherosclerotic arterial disease is essential for clinicians who manage patients with vascular disease.
Popliteal Entrapment Syndrome
Diagnostic Considerations
The popliteal entrapment syndrome is a developmental disorder resulting in an anomalous relationship between the popliteal artery and muscle structures in the popliteal fossa. Typical patients with popliteal entrapment are men (90%) younger than 30 years of age. The defect is bilateral in 20% to 30%. Patients initially present with typical symptoms of intermittent claudication. Loss of pedal pulses with dorsi and plantar flexion is frequently seen but nonspecific. The key to the diagnosis is cross-sectional imaging (CT, MRI) that shows the aberrant relationship between the popliteal artery and the gastrocnemius muscle.
Pathogenesis
Popliteal artery entrapment occurs as an abnormality during fetal development. The emergence of the popliteal artery as the dominant lower-extremity blood supply is preceded temporally by medial migration of the medial head of the gastrocnemius muscle that originally arises from the posterior fibula and lateral tibia. The numerous manifestations of popliteal artery entrapment occur as a result of aberrancies during this phase of development. The anomaly is typically not identified until adolescence or early adulthood. With repetitive injury, the popliteal artery becomes fibrotic and stenotic, and it ultimately thromboses.
Indications and Contraindications
Once diagnosed, all cases of popliteal artery entrapment should be repaired regardless of symptoms. The risk of subsequent arterial injury and ischemia in the young, healthy patient population in which this condition is found prohibits conservative management.
Anatomic Considerations
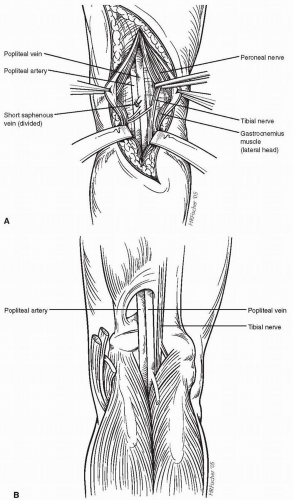
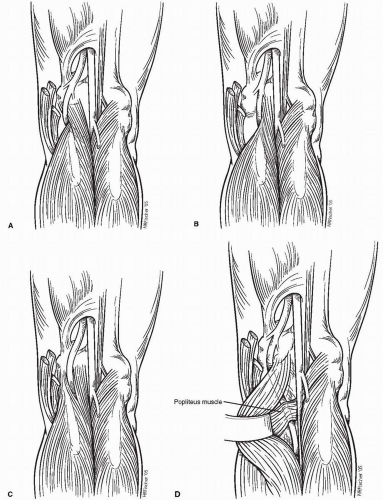
A thorough knowledge of the normal anatomy of the popliteal fossa is essential for the operative repair of popliteal artery entrapment (Figs. 53-1A and 53-1B). At least four anatomic variants are recognized. Type 1 (Fig. 53-2A) occurs in about 50% of the cases and is characterized by the medial deviation of the popliteal artery around the normally placed medial head of the gastrocnemius muscle. Type 2 (Fig. 53-2B) lesions (25%) involve an abnormal attachment of the medial head of the gastrocnemius with the popliteal artery passing medially but with less deviation than in type 1. In type 3 (Fig. 53-2C) (6%), the normally situated popliteal artery is compressed by muscle slips of the medial head of the gastrocnemius. Type 4 (Fig. 53-2D) lesions have associated fibrous bands of the popliteus muscle compressing the popliteal artery.
Pre-operative Assessment
Because most patients with popliteal artery entrapment are young and otherwise healthy, little pre-operative assessment is required once the diagnosis is made. If arterial repair with a vein graft is anticipated, it is worthwhile to perform pre-operative duplex saphenous vein mapping to identify the optimal site of vein harvest. Pre-operative contrast arteriography is useful in determining the degree of arterial stenosis or occlusion. This information is useful in planning the surgical repair, because stenotic or occluded arteries should be repaired with an interposition vein graft, while nonstenotic arteries may require only release from the compressive structures.
Operative Technique
The posterior approach to the popliteal artery is used most frequently for patients with popliteal entrapment because it allows clear delineation of the anatomic anomalies. If repair of the popliteal artery is anticipated, it is recommended to harvest the greater saphenous vein in the proximal thigh with the patient supine and then reposition the patient in the prone position after closing the harvest incision. Due to its larger size, the greater saphenous vein in the proximal thigh is preferred. Alternatively, the midportion of the saphenous
vein can be harvested with the patient in the prone position. Given the young age of afflicted patients and the known inferior patency of nonautogenous grafts in the lower extremities, the use of prosthetic grafts is discouraged.
vein can be harvested with the patient in the prone position. Given the young age of afflicted patients and the known inferior patency of nonautogenous grafts in the lower extremities, the use of prosthetic grafts is discouraged.
With the patient in the prone position and the knee slightly flexed, an incision is made in the popliteal fossa. Most authors have recommended an S-shaped incision to avoid scar contracture; however, others have used a straight, longitudinal incision without significant wound contracture. After dividing the subcutaneous tissue, the first structure encountered is the lesser saphenous vein. This is ligated and divided to facilitate further dissection. The deep fascia is then divided to enter the popliteal fossa. The sural nerve is identified immediately below the fascia and retracted laterally. The tibial nerve is the first major deep structure identified, with the peroneal nerve running more laterally and obliquely. Both nerves are gently retracted laterally. The stump of the lesser saphenous vein can be traced back to its origin from the popliteal vein, which is located deep in the popliteal fossa running longitudinally between the two heads of the gastrocnemius muscle. Under normal circumstances, the popliteal artery is adjacent and medial to the popliteal vein (Figs. 53-1A and 53-1B). In the case of popliteal entrapment (Figs. 53-2A-D), the compressing muscle is between these two structures, with the popliteal artery typically following a more medial course. The artery can be identified in the proximal popliteal space as it emerges from the adductor canal, with distal dissection clarifying the anatomic anomaly.
The repair of popliteal entrapment depends on the type of abnormality encountered. For type 1 lesions, in which the gastrocnemius muscle is in the correct anatomic position, the popliteal artery can be transected and either reanastomosed in the correct position between the two heads of the gastrocnemius muscle, or repaired with an interposition vein graft. Alternatively, and for lesions with abnormal muscle insertions, the compressing muscle is completely transected where it overlies the popliteal artery. The popliteal artery must be freed along its entire course. If the artery is otherwise normal, nothing further needs be done, although some have advocated reattachment of the medial head of the gastrocnemius muscle to the medial head of the femur where appropriate. More frequently, the artery will be severely fibrosed, stenotic, or occluded. Under these circumstances the artery should be repaired or replaced with an interposition graft.
The patient is systemically heparinized, and proximal and distal control are achieved with either silastic loops or vascular clamps. The abnormal portion of the artery is then resected. The normal proximal and distal popliteal arteries are spatulated to prevent anastomotic stenoses. The vein graft is spatulated and sewn in reversed orientation in an end-to-end configuration with running 5-0 or 6-0 monofilament vascular suture.
Complications and Postoperative Management
Injury to adjacent nerve and venous structures is rare with meticulous technique. Patients may begin ambulating the first postoperative day. Functional outcome, even with division of the medial head of the gastrocnemius muscle, is excellent. Potential peri-operative complications include bleeding, infection, graft thrombosis, and deep venous thrombosis (DVT). Duplex graft surveillance every 3 months for the first year and every 6 months thereafter is recommended per routine after lower-extremity bypass.
Cystic Adventitial Disease
Diagnostic Considerations
Adventitial cystic disease is a rare condition that, like popliteal artery entrapment, must always be considered in the differential diagnosis of claudication in young patients. Arterial stenosis is caused by single or multiple synovial-like cysts in the subadventitial layer of the arterial wall that compresses the arterial lumen. The cysts typically contain mucinous degenerative debris or clear, gelatinous material similar to that found in ganglia. Typical patients are men between the ages of 20 and 50 years old. The estimated incidence is 1:1,200 among patients with intermittent claudication. The popliteal artery is the most frequently involved artery, with the femoral and iliac arteries being the next most frequent areas of involvement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree