74 Treatment of Lipid Abnormalities
Diagnostic Approach
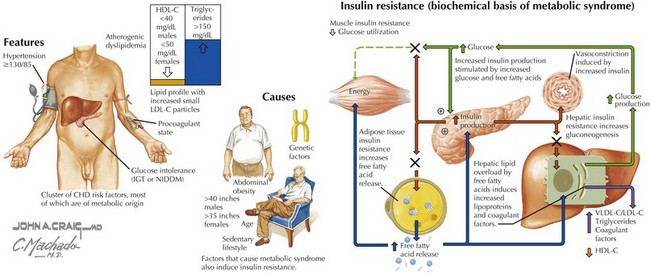
Lipid management requires the assessment of the patient’s short-term (10-year) risk for CHD events. The therapy and specific goals are then based on the patient’s absolute risk for a CHD event. The NCEP Adult Treatment Panel III recommends that patients with established coronary disease, diabetes, carotid artery disease, or lower extremity arterial disease be considered to be in the highest risk group (10-year risk >20%). Increasingly, metabolic syndrome and diabetes are becoming dominant cardiovascular risk factors, as the incidence of obesity in the United States and industrialized countries continues to increase (Fig. 74-1; see also Chapter 61). In the absence of such disease, patients’ global risk should be determined by the Framingham risk equation. Global risk is considered high if the 10-year risk is greater than 20%. The global risk of patients in the intermediate-risk (10-year risk of 10%–20%) and low-risk (10-year risk <10%) groups should be considered in light of the presence or absence of major CHD risk factors. The most important CHD risk factors are age (≥45 years for men, ≥55 years for women), a history of premature CHD in a first-degree relative, current cigarette smoking, the presence of hypertension, and HDL-C below 40 mg/dL. Patients with two or more major risk factors in addition to high LDL-C are considered to be at intermediate risk. Patients with one major risk factor in addition to high LDL-C are considered to be at low risk. Using the Framingham risk equation, the 20-year probability of the development of a CHD event can be estimated for patients with two or more risk factors. When the number of risk factors is 0 to 1, the Framingham scoring is not needed (see Chapter 11).