Fig. 6.1
Position of operative ports and liver retractor (Reprinted with permission)
Mobilization of the Distal Esophagus
An Allis clamp is inserted through Port D near the gastroesophageal junction to lift the gastrohepatic ligament, which is then divided. The esophagus is bluntly dissected from the right crus in order to access the posterior mediastinum. The posterior vagus nerve is identified. A Penrose drain is passed around the esophagus and both vagi, allowing for caudal retraction of the esophagus that will help deliver the diverticulum into the abdomen.
Exposure of the Diverticulum Neck
Once the diverticulum is located, it should be carefully dissected off the dense adhesions to the pleura and the esophageal wall. One must ensure the neck of the diverticulum is adequately isolated. In the case of a large diverticulum, one may need to divide the diaphragm anteriorly (Fig. 6.2). Care should be taken to mobilize the diverticulum neck completely, especially the most cranial portion. Failure to achieve this step may prompt to perform a myotomy and fundoplication transabdominally and then resorting to a thoracoscopic approach to complete the diverticular dissection and perform the final transection.
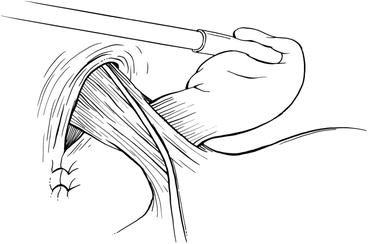
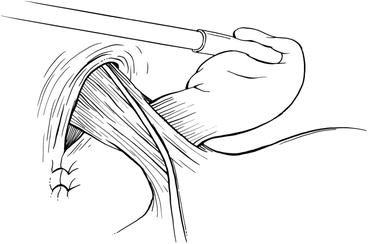
Fig. 6.2
A diverticulum is shown with its neck completely mobilized and its relationship with the anterior vagus nerve demonstrated. The hiatus has been already closed with two interrupted stitches (Reprinted with permission)
Stenting
After the diverticulum is dissected free and the neck is isolated, a 54–58 F bougie is inserted into the esophagus. The diverticulum is closed loosely with a grasper to prevent the bougie from entering it. An endoscope may be inserted into the esophagus as an alternative. Endoscopy also provides the option of inspecting and testing the integrity of the staple line after diverticulectomy.
Stapling
After the bougie is inserted past the diverticulum, a 2.5 mm vascular cartridge is inserted into the abdomen and oriented longitudinally to the esophagus. We pull back on the bougie prior to firing the stapler to avoid dragging the stent across the staple line. This minimizes staple line disruption. The bougie is then completely removed (Fig. 6.3).


Fig. 6.3
The stump of the neck of the diverticulum is shown after its stapled transaction alongside the esophagus (Reprinted with permission)
Esophageal Musculature Closure
The diverticulum is removed from the abdomen in a plastic bag. The muscular layers adjacent to the neck of the diverticulum are closed with interrupted sutures to reinforce the staple line (Fig. 6.4).
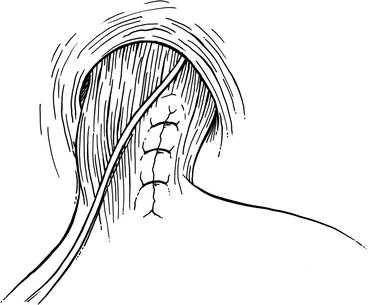
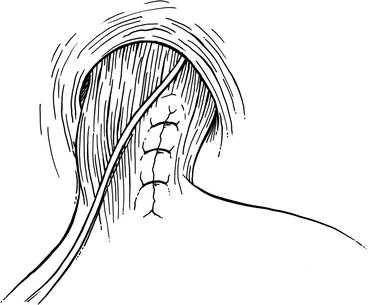
Fig. 6.4
The defect of the esophageal musculature is closed in one layer with interrupted sutures to imbricate the staple line (Reprinted with permission)
Myotomy
The myotomy is performed contralateral to the site of the resected diverticulum. It is extended 7 cm cranially proximal to the cranial extent of the diverticulum and 3 cm caudally onto the anterior wall of the stomach until the first branch of the left gastric artery is identified (Fig. 6.5). The anterior vagus nerve is preserved during the myotomy.
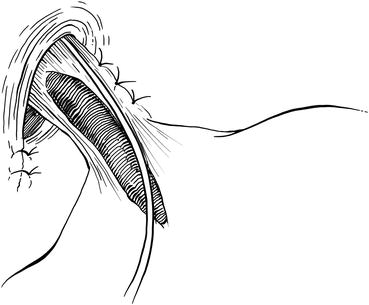
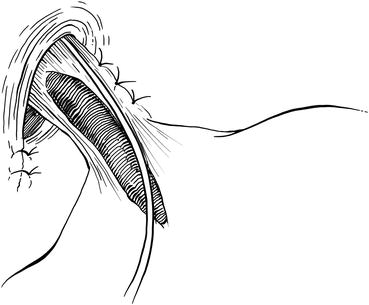
Fig. 6.5
A contralateral myotomy is shown extending onto the body of the esophagus and onto the anterior wall of the stomach. The myotomy is 10 cm long and it is located at the 10 o’clock position (Reprinted with permission)
Closure of the Esophageal Hiatus
Heavy silk interrupted sutures are used to close the hiatus. To avoid postoperative dysphagia from constriction of the esophageal and prevent a leak at the staple line due to outflow obstruction, the uppermost crural stitch is placed 1 cm posterior to the esophagus. If the diverticulum was large and required anterior splitting of the diaphragm, this is now closed with 0-0 silk interrupted sutures.
Partial Fundoplication
A partial anterior (Dor) fundoplication is preferred and prevents reflux after the myotomy. The short gastric vessels may be divided to enable a tension-free fundoplication. The gastric fundus is then sutured laterally to the apex of the left crus and the left edge of the myotomy. The stomach is folded over the myotomy. It is sutured superiorly along the diaphragmatic hiatus and medially along the right crus with interrupted sutures (Fig. 6.6).
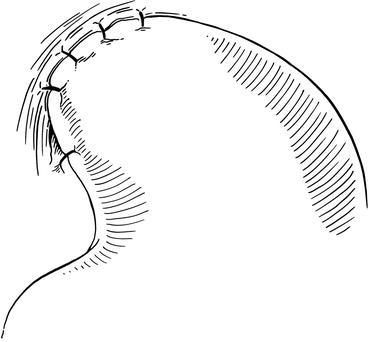
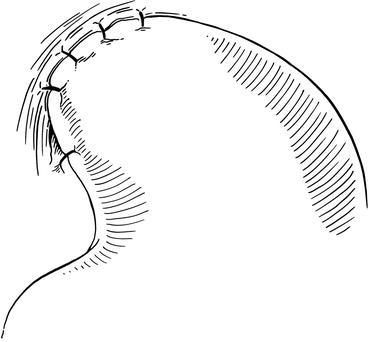
Fig. 6.6
Completed partial anterior fundoplication (Reprinted with permission)
Upon completion of the operation, the Foley catheter is removed while the patient is still in the operating room. The patient is admitted overnight. On postoperative day 1, some surgeons perform a contrast swallow study to evaluate for a possible leak. If no leak is present, the patient is advanced to a soft mechanical diet which he or she will maintain for 1 week postoperatively. The patient will then follow-up in clinic and have dietary restrictions lifted at that time.
Technique of Thoracic Repair
Preparation
The patient undergoes general anesthesia and a double-lumen endotracheal tube is inserted. Perioperative antibiotics are administered, and venous thromboembolic prophylactic measures are instituted, including lower extremity pneumatic compression devices and subcutaneous heparin. The patient may be placed in either the right (left side up) or left (right side up) lateral decubitus position, depending on the location and orientation of the diverticulum. Most often, pulsion diverticula present to the right side, and so a right thoracic approach is generally favored. Others may prefer a left-sided approach, especially for diverticula that present to the left. The choice is only moderately important, as circumferential dissection of the esophagus is often needed to both treat the diverticulum and perform a subsequent myotomy away from the site of diverticulectomy. The ipsilateral lung is deflated.
Port Placement
The surgeon may stand facing the patient’s back or chest, according to personal preference. This chapter describes an approach used when the surgeon stands at the patient’s back. Access is gained through a 5 mm camera port low in the chest in the posterior axillary line, two working ports anterior and posterior to the camera port, and a 3 cm non-rib spreading access incision placed anterolaterally in the 4th interspace. Ports are positioned with the goal of having the target in line with the camera and between the two working ports (Fig. 6.7). The pleural cavity may be insufflated initially with warm, humidified carbon dioxide at a pressure of 8 mmHg to facilitate lung deflation. A suture may be placed through the central tendon of the diaphragm and brought out through the lower anterior chest wall to improve visualization.
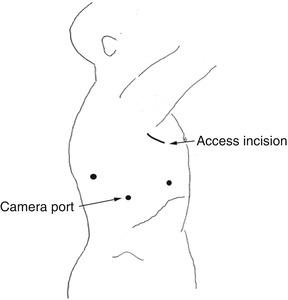
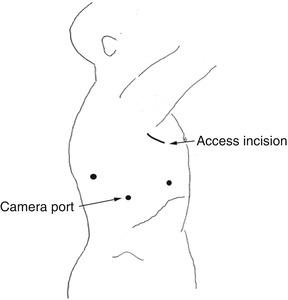
Fig. 6.7
Port placement for thoracoscopic esophageal diverticulectomy and myotomy
Esophageal Mobilization
The site of the diverticulum is identified. The mediastinal pleura overlying the diverticulum and the adjacent esophagus is incised. The esophagus is mobilized with a sealing device (EnSeal™ or Ligasure™), hook-electrocautery, or scissors. Mobilization should be sufficient to permit exposure of the neck of the diverticulum. In addition, exposure of the wall of the esophagus 90–180° circumferentially from the diverticulum and from proximal to the neck of the diverticulum to the gastroesophageal conjunction is necessary to perform the myotomy. Care should be taken to avoid injury to the vagus nerves, which should be clearly identified. A Penrose drain may be used to encircle the adjacent esophagus to facilitate retraction and mobilization.
Dissection of the Diverticulum
The diverticulum is bluntly and sharply dissected free from the surrounding structures. It is important to dissect the investing connective tissue from the diverticulum, revealing its origin from between the split fibers of the esophageal circular and longitudinal smooth muscle layers.
Stenting the Esophagus
After the diverticulum is sufficiently dissected, an assessment is made as to whether resection of the diverticulum is needed. Small, wide-mouthed diverticula may be left in situ, eliminating a risk of perforation or suture line breakdown. In most patients, however, diverticulectomy is appropriate. A 48–50 Fr bougie is passed to prevent excess mucosa from being excised during the diverticulectomy. Care must be taken to prevent bougie entry into the diverticulum, which could result in inadvertent perforation. Alternatively, an endoscope may be used to stent the esophagus while the diverticulectomy is performed.
Diverticulectomy
An endostapler is positioned at the base of the diverticulum and parallel to the esophagus (Fig. 6.8). Care should be taken to gently retract the diverticulum during stapler firing but not to pull it too tightly. More than one firing of the stapler may be used in sequence; care should be taken to ensure that they are in line with each other. The specimen is retrieved through the access port. The continuity of the mucosa should be assessed by direct inspection thoracoscopically and endoscopically during air insufflation.
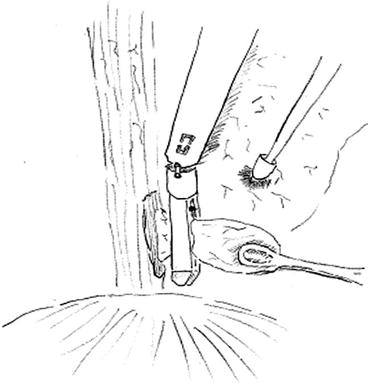
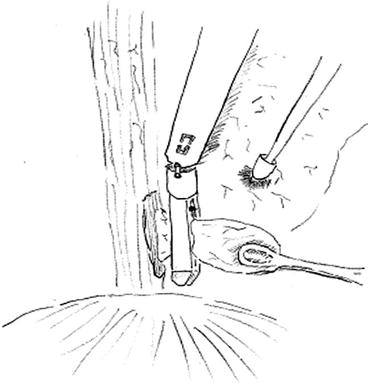
Fig. 6.8
Placement of the endostapling device for thoracoscopic diverticulectomy (Note: The stapler is place through the access incision. The dark area at the base of the diverticulum represents the cut muscle. There is a push retracting the lung anteriorly)
Muscle Approximation
The muscular layers over the mucosa are approximated with running or interrupted absorbable suture. This reinforces the staple line and helps prevent contamination of the pleural space should a small leak from the stable line occurs.
Myotomy
The esophagus is rotated 90–180° away from the site of the diverticulectomy. Dilute epinephrine may be injected submucosally along the line of the planned myotomy to hydrodissect the plane and to constrict the submucosal plexus of vessels that may otherwise cause annoying bleeding. The myotomy is performed using hook-electrocautery, scissors, or EnSeal, extending from proximal to the diverticulum origin and extending inferiorly. For very distal diverticula, the myotomy should extend through the lower esophageal sphincter. Leaving the hiatus intact provides sufficient antireflux effect, making a fundoplication unnecessary. For most diverticula, especially those without a defined abnormality on manometry such as achalasia, diffuse spasm, or nutcracker esophagus, the myotomy can end just at the lower esophageal sphincter. Endoscopic insufflation is performed again to ensure that no mucosal injury has occurred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


