Fig. 1.1
Layers in the esophageal wall
Contrary to the rest of the gastrointestinal tract, the esophagus has no serosal layer.
Blood Supply
The cervical portion of the esophagus is supplied by branches of the inferior thyroid arteries. The upper thoracic portion receives blood from the bronchial arteries, while the midthoracic portion is nourished by esophageal branches that arise directly from the aorta. The intercostal arteries may also contribute. The lower thoracic portion and diaphragmatic and abdominal segments are supplied by the left inferior phrenic artery and by the esophageal branches of the left gastric artery (Fig. 1.2).
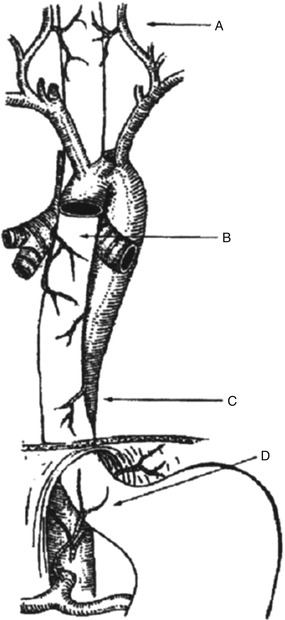
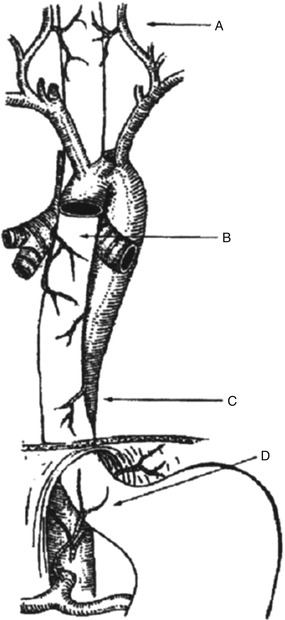
Fig. 1.2
Arterial blood supply to the esophagus. A inferior thyroid artery, B bronchial artery, C aorta, D left gastric artery
The submucosal venous drainage is more complex and variable. The veins that drain the cervical esophagus are tributary of the inferior thyroid veins; the veins from the thoracic esophagus drain into the hemiazygos and azygos veins. The most important veins are those that drain the lower esophagus. Blood from this region passes into the esophageal branches of the coronary vein, which is a tributary of the portal vein.
Lymphatic Drainage
Abundant lymphatic vessels form a dense submucosal plexus. Lymph usually flows longitudinally, running proximal in the upper two thirds and distal in the lower third of the esophagus. Lymph from the cervical esophagus drains mostly into the cervical and paratracheal lymph nodes, while lymph from the lower thoracic and abdominal esophagus reaches preferentially the retrocardiac and celiac nodes. However, the drainage is not segmental; therefore, lymph can flow for a long distance in the plexus before crossing the muscular layer and reaching the paraesophageal lymph nodes [2].
The thoracic duct originates from the cisterna chyli that is located in the abdomen, at the level of the second lumbar vertebra. The duct enters the chest through the aortic hiatus and runs in the posterior mediastinum to the right of the midline between the esophagus and the azygos vein. At the level of the fifth thoracic vertebra, it crosses the midline behind the esophagus and reaches the base of the neck. Then, it curves to the right to drain into the internal jugular vein. A single thoracic duct is described in about 70 % of people, while two or more are present in the remainder individuals [3] (Fig. 1.3).
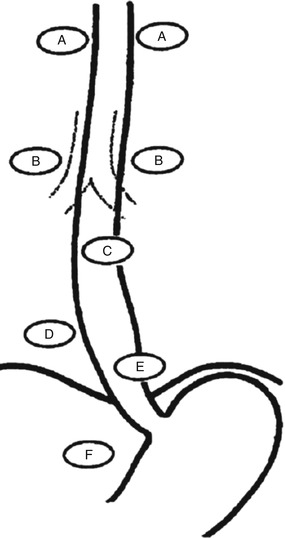
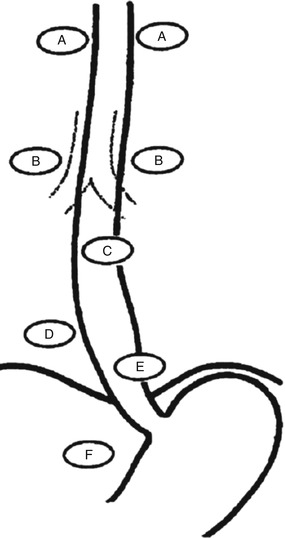
Fig. 1.3
Lymphatic drainage of the esophagus. A internal jugular nodes, B tracheobronchial nodes, C periesophageal nodes, D posterior mediastinal nodes, E retrocardiac nodes, F celiac nodes
Innervation
The striated muscle of the pharynx and upper esophagus is innervated by fibers that originate in the brain stem at the level of the nucleus ambiguus. The distal esophagus and LES receive nerves that originate in the dorsal motor nucleus of the vagus and end in ganglia in the myenteric plexus. The myenteric plexus is located between the longitudinal and the circular muscle layers and receives efferent impulses from the brain stem and afferent impulses from the esophagus. Two main types of effector neurons are found in this plexus: (1) excitatory neurons and (2) inhibitory neurons that mediate contraction of the musculature via cholinergic receptors and via vasoactive intestinal polypeptide and nitric oxide.
The vagus nerves run along each side of the neck until they reach the thoracic esophagus, where they form an extensive plexus. Above the diaphragm, they form two trunks [4]. The left trunk runs anterior while the right trunk is more posterior once they cross the esophageal hiatus. The anterior vagus then divides and gives rise to the hepatic branch and the anterior nerve of Latarjet, while the posterior vagus gives rise to the celiac branch and the posterior nerve of Latarjet. The posterior nerve of Latarjet runs parallel but deeper to the anterior counterpart in the gastrohepatic ligament about 1 cm from the lesser curvature of the stomach.
Branches of the superior and inferior cervical ganglia in the neck, the splanchnic nerves, and the celiac plexus in the chest and in the abdomen provide the sympathetic innervations. These nerves do not have a motor function and mainly modulate the activity of other neurons.
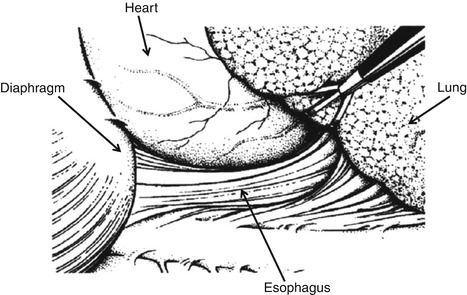
Right Thoracoscopic View
The thoracoscopic approach to the right chest provides an excellent view of the esophagus from the thoracic inlet to the gastroesophageal junction (Fig. 1.4). The camera is usually inserted in the sixth intercostal space. In order to obtain adequate exposure, the right lung is deflated and retracted anteriorly, while the inferior pulmonary ligament is divided. After incision of the mediastinal pleura, most thoracic esophagus is exposed. The upper thoracic part of the esophagus is crossed anteriorly by the right brachiocephalic vessels. At the level of the right main stem bronchus, the azygos vein passes from a paravertebral position anteriorly to enter the superior vena cava, crossing over the esophagus [5]. Distal to the inferior pulmonary vein, the esophagus lies between the heart and the descending aorta. The sympathetic chain and ganglia run vertically, parallel and lateral to the azygos vein, crossing over the intercostal vessels.
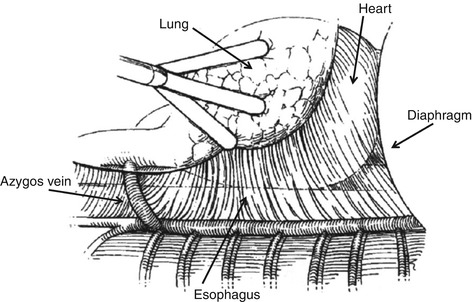
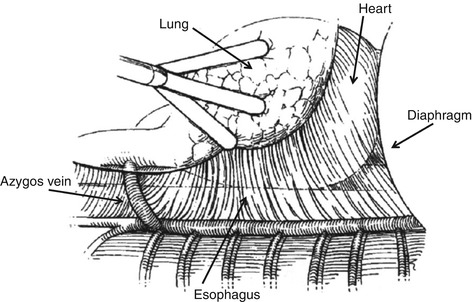
Fig. 1.4
Right thoracoscopic view
Left Thoracoscopic View
Left thoracoscopy provides a good view of the esophagus from the aortic arch to the gastroesophageal junction (Fig. 1.5) [6]. The camera is usually inserted in the sixth intercostal space. After deflation and anterior retraction of the lung, the inferior pulmonary ligament is divided and the mediastinal pleura opened. The esophagus can be identified in the space between the pericardium and the descending aorta. Behind and lateral to the aorta, the hemiazygos vein runs along the anterolateral aspect of the vertebral bodies, draining the left intercostal veins. It crosses behind the esophagus to join the azygos vein on the right at the level of the eighth thoracic vertebra.