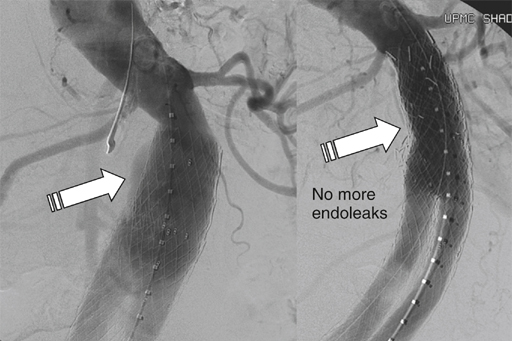
There are five major categories of endoleaks (Table 1). Some appear to be an unavoidable consequence of placing a stent graft inside an aneurysm sac with patent outflow vessels, some are the result of poor seal at the proximal or distal fixation sites or between the graft components, and others occur as a result of graft material failure. Endoleaks are associated with a variable increase in intrasac pressure that depends on the type of endoleak, which determines its severity and clinical significance. TABLE 1 Classification of Endoleaks and Endotension Late type I endoleaks can occur as a result of graft migration, aneurysmal degeneration of the aortic neck, enlargement of the iliac arteries, or severe angulation at the fixation site that can disengage the stent graft from the aortic wall as the sac starts to shrink. The treatment of late type I endoleaks can be more challenging, but it usually also involves ballooning, stent graft extension (Figure 1), or use of Palmaz stent to increase the graft radial force and apposition to the aortic wall.
Treatment of Endovascular Leaks After Aortic Endografting
Endoleak Type
Source of Perigraft Flow
I
Attachment site
Ia
Proximal, aortic end
Ib
Distal, iliac end
Ic
Iliac occluder
II
Branch leaks
IIa
Simple: one patent branch
IIb
Complex: two or more patent branches
III
Stent graft defect
IIIa
Junctional leak or modular disconnect
IIIb
Fabric holes
IV
Stent graft porosity <30 days after implantation
Primary endoleak
Present from the time of EVAR
Secondary endoleak
Diagnosed after a prior negative CTA
Endotension
AAA enlargement with increased intrasac pressure after EVAR with no endoleak on CTA
Type I Endoleak
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


