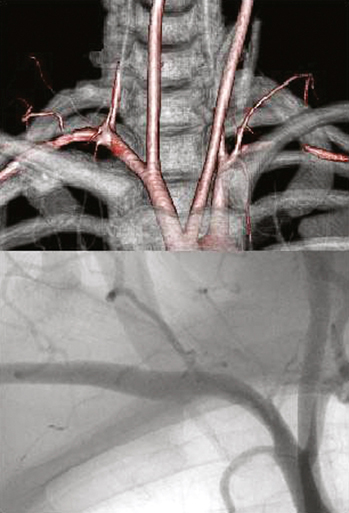
Complete cervical ribs typically elevate the floor of the thoracic outlet, significantly increasing the compression of the subclavian artery by the anterior scalene muscle (Figure 1). Cervical ribs are found in less than 0.5% of the general population, and are twice as common in women as in men. Their presence is associated with histopathologic changes in the brachial plexus, including fibrosis, vascular hyalinization, mucinous degeneration, and intraneural collagen nodules. Changes are not seen in nerve specimens of patients without cervical ribs. This observation suggests that in cases of arterial compression by a cervical rib, nerve compression is likely also present. The pathologic vascular changes that occur in patients with arterial TOS are progressive and can be classified in stages. Stage 1 patients have severe or complete arterial obstruction seen only with positional changes of the upper extremity, typically with arm abduction and external rotation, with the artery appearing normal in neutral position. Stage 2 patients experience arterial changes in the neutral position in the form of mild poststenotic dilatation, fixed stenosis, or luminal irregularities. Stage 3 patients have true arterial aneurysms or with complete occlusion of the subclavian or axillary arteries (Figures 2 and 3). Although it is unusual, some patients with axillary artery compression have aneurysms at the origin of the circumflex humeral arteries.
Treatment of Arterial Complications in Thoracic Outlet Syndrome
Anatomic Features

Clinical Presentation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
