30 Transradial Percutaneous Coronary Intervention for Major Reduction of Bleeding Complications
Both diagnostic coronary angiography and PCI are most commonly performed via the trans-femoral access in a majority of catheterization laboratories. Initial reports in the late 1980s demonstrated the feasibility and security of diagnostic coronary angiography via the trans-radial approach.1 The development of highly active anti-thrombotic regimens associated with a major reduction of thrombotic complications of PCI, in part resulting in a significant increase in femoral access site–related bleeding complications, led to the development of the trans-radial approach to PCI in the past decade. The use of 6F and more recently 5F guiding catheters, with the generalization of 6F-compatible or 5F-compatible balloons, coronary stents, and other approaches such as rotational atherectomy, thrombectomy, or distal protection devices allow treatment of complex lesions, for example, multi-vessel PCI, bifurcation lesions, and so on. These approaches are used in complex situations such as PCI for acute coronary syndrome (ACS), including primary or rescue PCI via the trans-radial approach, following a relatively short and easy learning curve. Although still used rarely in the United States (1.3% of procedures), the use of PCI via the trans-radial approach is growing to an impressive extent in Asia and Europe as was recently reported.2 In the setting of ACS more than 80% of procedures were performed through the radial access.3 Similarly primary PCI is more and more frequently performed through a radial access as recently shown in the international randomized ATOLL study, where 66% of procedures used the radial artery.4
 Rationale for the Trans-Radial Approach
Rationale for the Trans-Radial Approach
Feasibility
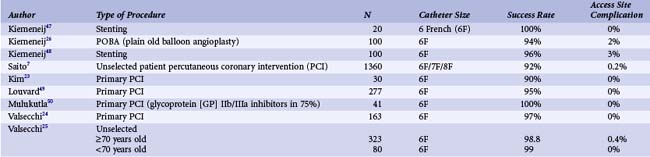
The feasibility and security of the trans-radial approach to coronary diagnostic or interventional procedures have been widely demonstrated. Data from such studies are summarized in Table 30-1. Even in the case of experienced operators, the trans-radial approach requires a learning curve to achieve higher rates of procedural success and shorter duration of the procedure and x-ray exposure.5 Overall, the feasibility of the trans-radial approach for diagnostic or interventional coronary procedures is high (>90%), especially in experienced centers (>95%). In a series of 1119 consecutive patients in South Korea, the mean radial artery diameter measured by ultrasound was 2.6 ± 0.41 mm in men and 2.43 ± 0.38 mm in women.6 In another series of 250 patients in Japan, the radial artery diameter was larger than 7F and 8F catheters in 71.5% and 44.9% of male patients and 40.3% and 24% of female patients respectively.7 Although such data may not be totally generalizable to all other populations, they underscore the fact that the trans-radial approach could potentially be used in a majority of patients with 5F, 6F, and even 7F catheters. In some patients with sufficiently large artery diameters, 8F catheters may also be used, if needed. The trans-radial approach has been used for different types of procedures with various devices such as intravascular ultrasound (IVUS)–guided stenting, coronary brachytherapy, distal protection, embolectomy, rotational atherectomy, myocardial biopsy, and bifurcated stents. The approach is incompatible with the intra-aortic balloon pump and all other devices or procedures that need larger than 8F access. Recently, the use of sheathless guiding catheters, with smaller outer diameters—6.5F and 7.5F catheters with introducers of less than 5F and 6F diameters, respectively—has been reported to be feasible and safe. Although their use is infrequent, such catheters may allow complex procedures such as simultaneous kissing stenting.
 The Trans-Radial Approach Versus the Trans-Femoral Approach for PCI
The Trans-Radial Approach Versus the Trans-Femoral Approach for PCI
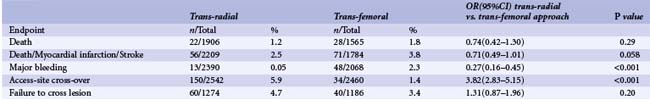
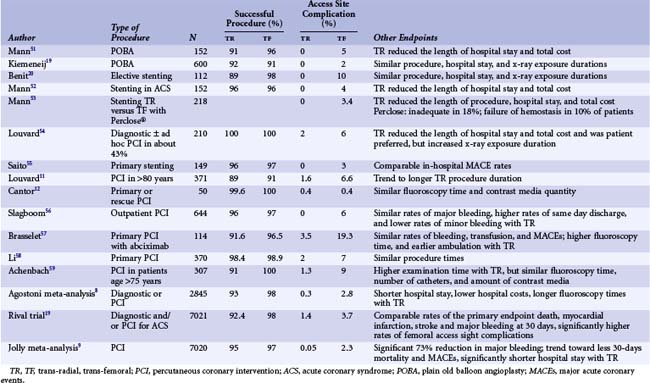
Compared with the trans-femoral approach, the trans-radial access is associated with fewer vascular complications, more comfort for patients, the possibility of rapid ambulation, less procedure cost, and shorter hospital stay. Several randomized trials comparing the advantages and disadvantages of each method are summarized in Table 30-2. A meta-analysis of 11 published and unpublished randomized controlled trials, which included 3224 patients, showed that the overall rates of postprocedure major ischemic coronary events are comparable in both methods, the procedural success rate is higher with the trans-femoral approach (98% vs. 93%, P = 0.0009), and all of these studies and the pooled analysis demonstrated the significant advantage of the trans-radial approach in terms of bleeding complications, mainly an 89% risk reduction for entry site complications (0.3% vs. 3%, P < 0.0001).8 The previous meta-analysis also showed a clear ongoing trend toward equalization of procedural success rates between the two approaches through the years. Such finding is probably explained by technologic advancements in materials and improvement in operators’ skills and experience following the learning curve. The average duration of exposure to x-ray was, nevertheless, longer for the trans-radial approach (8.9 vs. 7.8 minutes, P < 0.001). Another, more recent meta-analysis of 23 published and unpublished randomized trials, which included 7020 patients undergoing coronary angiography or PCI concordantly, showed a significant reduction (73%, P < 0.001) in the rate of major bleeding in those undergoing PCI as well as a trend toward lower rates of the combined endpoint of death, myocardial infarction (MI), or stroke (odds ratio [OR] 0.71, P = 0.058) and death (OR 0.74, P = 0.29). The major findings of the study are summarized in Table 30-3. Although access site cross-over was higher in the trans-radial approach, the procedure failure rate was not significantly lower and was particularly similar among operators who preferred the trans-radial approach, and there was a trend toward higher failure (P = 0.07) among less experienced operators. Such advantages make the trans-radial approach the method of choice for outpatient PCI, which has been reported to be highly feasible and safe. The trans-radial approach is also of particular interest with regard to patients at high risk for bleeding (older adults, women, patients with renal failure, obese persons, or patients on multiple anti-thrombotic agents, especially glycoprotein [GP] IIb/IIIa inhibitors); for example, it has been reported to be associated with fewer vascular complications in obese patients (multivariate OR 0.12; 95% confidence interval [CI] 0.02–0.94, P = 0.043) in a retrospective series of 5234 diagnostic or interventional (56.6%) procedures, as well as in older adults (1.6% vs. 6.5%, P = 0.03).10,11 Other patients who benefited from the obvious advantages of the radial approach over the femoral approach are those with severe peripheral arterial disease (PAD), proximal PAD, or both; patients with bilateral aorto-femoral bypass graft; patients with aortic aneurysms; and patients with a prior history of femoral complications after catheterization. The trans-radial approach is also of particular interest in the setting of primary PCI (see Tables 30-1 and 30-2) performed by experienced operators in patients treated with aggressive anti-thrombotic regimens, in whom life-threatening access-site bleeding complications and the subsequent MACEs may be avoided with the trans-radial approach. In such a setting, there is growing evidence that the trans-radial approach is associated with overall similar door-to-balloon times, lower rates of vascular complications and bleeding in the presence of triple anti-platelet therapy, and even reduced 30-day mortality compared with the femoral approach.12–16 It may also be of interest in patients with chronic kidney disease, as in the British Columbia cohort of 69,214 patients who underwent catheterization. Compared with the radial access, the femoral access was associated with an adjusted odds ratio of 4.36 (2.48–7.66) for the development of the composite endpoint of new dialysis or new chronic kidney disease.17 Such findings may be related to the reduced risk of atheroembolism in the trans-radial approach. Finally, when considering recent PCI registries such as the RIVIERA (Registry on IntraVenous anticoagulation In the Elective and primary Real world of Angioplasty) registry, which prospectively included 7962 unselected patients, the trans-radial approach appeared as an independent predictor of better in-hospital outcome (OR for death or MI 0.16; CI 0.05–0.50) as well as the only variable correlated to less bleeding.18 Similar results were also reported by the Canadian MORTAL (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg) registry; which included 38,872 procedures (20.5% by the trans-radial approach); this registry showed a significant reduction of 30-day mortality (adjusted OR 0.71; CI 0.61–0.82) and 1-year mortality (adjusted OR 0.83; CI 0.71–0.98) by the latter approach. The superiority of the trans-radial approach in the prior study appears to be entirely linked to the reduced rates of transfusion. The major study comparing the trans-radial and trans-femoral approaches is the very recently published RIVAL trial.18a The RIVAL trial included in 7021 ACS patients randomly assigned to each of the approaches for angiography and/or PCI. Indications for angiography were STEMI in 27.2% and 28.5% and NSTEMI in 28.5% and 25.8% in trans-radial and trans-femoral groups respectively. Angiography was performed in 99.8% and PCI in approximately 66% of patients in both groups. PCI success rates were comparable between the 2 groups (95.4% versus 95.2%), with higher access site crossover rates in the transradial group (7.6% versus 2%, P < 0.0001). The rates of primary endpoint the composite of death, myocardial infarction, stroke, or non-CABG bleeding at 30 days occurrence were comparable between the trans-radial and trans-femoral groups (3.7% and 4%), as well as each of the individual components. However the secondary endpoint of major vascular complications occurred more often in the trans-femoral group (1.4% versus 3.7%, P < 0.0001). Moreover all post-hoc exploratory outcomes including ACUITY-defined major bleeding, the composite of death, myocardial infarction or ACUITY major bleeding, and the composite of major non-CABG bleeding and vascular complications were more frequent in the trans-femoral group.
TABLE 30-2 Randomized Trials Comparing Trans-radial and Trans-femoral Approaches for Percutaneous Coronary Intervention
 The Trans-Radial Approach Versus the Trans-Brachial Approach
The Trans-Radial Approach Versus the Trans-Brachial Approach
Two of the randomized trials mentioned above also included a group of patients who underwent PCI through the trans-brachial approach. The ACCESS study reported comparable procedural success rates, equipment consumption, and procedural and fluoroscopy times among the three approaches for PCI.19 The trans-brachial approach was associated with higher rates of vascular complications compared with the trans-radial approach (2% vs. 0%, P = 0.035). The BRAFE (Brachial, RAdial, or Femoral approach for Elective Palmaz-Schatz stent) study compared the trans-radial and trans-femoral approaches to a trans-brachial cut-down approach and reported no local vascular complication with the latter approach.20 Such brachial approach is not commonly used and appears unacceptably aggressive. The brachial access does not need a cut-down and can be obtained with a classic percutaneous approach; but the brachial access is usually preferred when neither femoral nor radial approaches are possible.
 The Trans-Radial Approach Versus the Trans-Ulnar Approach
The Trans-Radial Approach Versus the Trans-Ulnar Approach
The PCVI-CUBA (22) study randomized 413 patients with a normal direct or reverse Allen’s test to undergo coronary angiography with or without subsequent PCI through the trans-radial approach versus the trans-ulnar approach. The two methods were associated with similar rates of access success (96% vs. 93%), PCI success (96% vs. 95%), and asymptomatic access-site artery occlusion (5% vs. 6%) rates.21 Vascular complications occurred only in two patients in the trans-ulnar group. If confirmed by further data, the trans-ulnar approach would be an alternative to the trans-radial approach for PCI, although the ulnar artery is usually less superficial and its compression may be little more difficult technically.
 Cost-Effectiveness
Cost-Effectiveness
Although based on small studies, there is systematically concordant evidence that because of shorter hospital stay, reduced nursing workload, reduced rates of complications, and absence of need for closure devices, the trans-radial approach is associated with significant cost reduction in both diagnostic angiography and PCI settings.22
 Practical Considerations for the Trans-Radial Approach
Practical Considerations for the Trans-Radial Approach
Assessment of Ulno-palmar Arterial Arches
Classically, the assessment of collateral ulnar circulation is recommended before undertaking the trans-radial approach to PCI. Early postprocedure occlusion of the radial artery could occur in 0% to 19% of patients, depending on the clinical or ultrasound assessment of the patency of the radial artery, the diagnostic or interventional type of procedure, whether or not anticoagulation is used, and the size of the catheters.7,23–25 In 40% to 60% of cases, the pulse could be re-detected within hours to weeks after the occlusion, which remains asymptomatic in virtually all patients.26,27 Nevertheless, incomplete palmar arches and very rare cases of transient or definitive hand or finger ischemia have been reported, which justifies the evaluation of the ulno-palmar arch before the radial puncture. Although assessment of the collateral ulnar circulation is recommended, the low specificity of Allen’s test and the absence of symptomatic ischemic complications in the abundant literature have made this recommendation obsolete in many experienced radial centers.
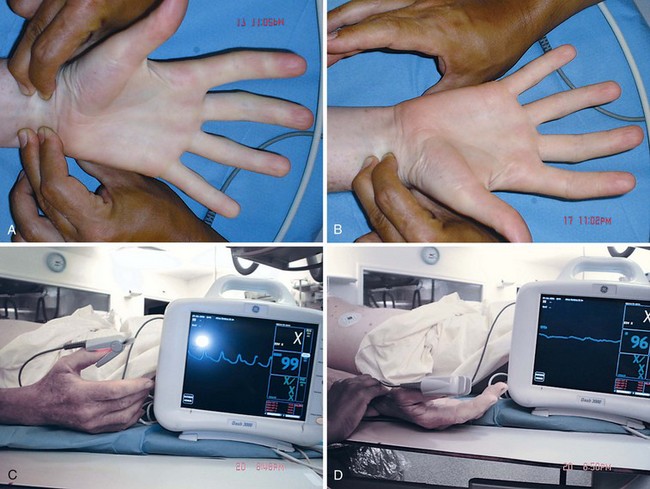
Allen’s Test
A simple way of testing the adequacy of the collateral ulnar circulation clinically is the modified Allen’s test (Fig. 30-1). The test consists of the simultaneous compression of radial and ulnar arteries, followed by several flexion–extension movements of fingers, which would lead to loss of color in the palm. The ulnar compression is then removed. The re-coloration time of the palm after removal of the ulnar artery compression defines Allen’s test: normal less than 5 seconds, intermediate 5 to less than 10 seconds, abnormal 10 seconds or more. The reverse Allen’s test comprises all of the above steps except that transient radial compression instead of ulnar compression could be used with the trans-ulnar approach. In clinical practice, the trans-radial approach could be attempted in normal or intermediate patient groups. While the prognostic relevance of Allen’s test is still being debated, a recent study demonstrated reduced blood flow and increased capillary lactate levels in the thumb following 30-minute occlusive compression of the radial artery in patients with abnormal result of Allen’s test compared with those with a normal result.28 Although such findings are suggestive of potential ischemic complications in patients with abnormal results, the association with the safety of the procedure has never been shown.