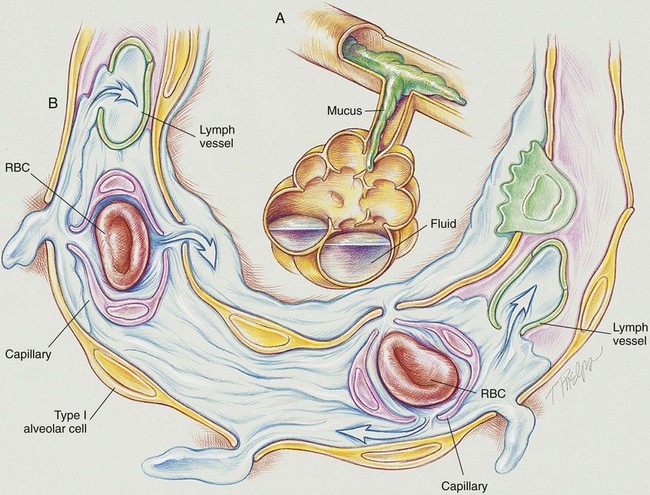
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with transient tachypnea of the newborn. • Describe the causes of transient tachypnea of the newborn. • List the cardiopulmonary clinical manifestations associated with transient tachypnea of the newborn. • Describe the general management of transient tachypnea of the newborn. • Describe the clinical strategies and rationales of the SOAP presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. Transient tachypnea of the newborn (TTN) (also called type II respiratory distress syndrome and “wet lung” syndrome) was first described in the literature in 1965. Within the first 4 to 6 hours after birth, TTN produces clinical signs very similar to those associated with the early stages of respiratory distress syndrome (see Chapter 34). However, the anatomic alterations of the lungs associated with TTN are much different from the pulmonary pathology seen in respiratory distress syndrome. As shown in Figure 33-1, the infant with TTN has a delay in the pulmonary fluid absorption by the lymphatic system and pulmonary capillaries. It is thought that this condition results, in part, from the infant’s hypoxemia and inadequate inspiratory effort, producing a delay in clearance of pulmonary fluid. As this condition worsens, the infant develops pulmonary capillary congestion, interstitial edema, decreased lung compliance, decreased tidal volume, and increased dead space. Because the swallowing and cough efforts of infants with TTN are commonly depressed, the clearance of bronchial secretions is compromised. This condition often leads to air trapping and alveolar hyperinflation. The major pathologic or structural changes associated with TTN are as follows:
Transient Tachypnea of the Newborn
Anatomic Alterations of the Lungs