Stroke is a devastating complication after transcatheter aortic valve implantation (TAVI) and might partially be related to cardiac embolization. The aim of this single-center prospective study was to determine the incidence of intracardiac thrombi and left atrial spontaneous echo contrast (SEC), both known predictors of cardiac embolic stroke, in patients referred for potential TAVI. One hundred four consecutive patients with severe symptomatic aortic valve stenosis and at high or very high risk for surgery were included and underwent transesophageal echocardiography. In 11 patients (10.6%), intracardiac thrombi were detected, and 25 patients (24%) showed dense grade 2 SEC. Atrial fibrillation (p <0.0001), diastolic dysfunction (p = 0.0005), and atrial size (p = 0.0038) were related to the presence of intracardiac thrombus and/or dense SEC on multivariate analysis. In conclusion, the incidence of intracardiac thrombi and dense SEC in (very) high-risk patients with severe aortic valve stenosis referred for potential TAVI is high and can accurately be detected using transesophageal echocardiography. Systematic thromboembolic evaluation using transesophageal echocardiography is thus recommended in patients referred for TAVI.
Transcatheter aortic valve implantation (TAVI) is now considered the standard of care in patients at very high surgical risk with symptomatic severe aortic valve stenosis and as an alternative to surgery in those considered at high risk. Periprocedural and early postprocedural transient ischemic attack (TIA) and stroke, however, remain major and devastating complications with significant impact on quality of life and long-term survival. The pathophysiologic mechanisms leading to neurologic events after TAVI are multiple and related to embolic but also to nonembolic phenomena, such as systemic hypotension during valve implantation. Intracardiac thrombi and dense spontaneous echo contrast (SEC) in the left atrium are well-known risk factors for cardiac embolic stroke and can accurately be detected using transesophageal echocardiography (TEE). Their presence is influenced by atrial fibrillation, age, associated co-morbidities, elevated filling pressures, and valvular disease. The incidence of intracardiac thrombi and SEC, specifically in (very) high-risk patients with multiple co-morbidities, severe aortic valve stenosis, and referred for potential TAVI, however, is not well documented.
Methods
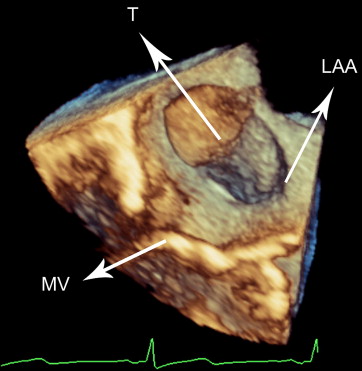
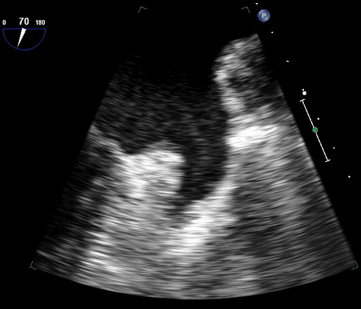
The prespecified aim of this prospective single-center study was to determine the incidence of intracardiac thrombi and left atrial SEC using TEE in consecutive (very) high-risk patients with severe aortic valve stenosis referred for potential TAVI, to reduce procedural stroke and TIA. Patient characteristics, systolic and diastolic left ventricular function, associated valvular disease, flow velocities in the left atrial appendage (LAA), presence of (paroxysmal or continuous) atrial fibrillation, and use of antithrombotic therapy were registered. The primary end point of this study was the incidence of intracardiac thrombi and dense SEC. The presence of an intracardiac thrombus ( Figure 1 ) was a contraindication for TAVI at our center, and antithrombotic therapy was intensified or started for ≥6 weeks. TAVI could be performed only after complete thrombus disappearance. SEC, however, was not considered a contraindication for eventual TAVI. Because procedure-related stroke and TIA occur mainly within first month after TAVI, 1-month stroke and TIA incidence was assessed. Stroke and TIA were defined according to the Valve Academic Research Consortium definitions.
The study was designed by the investigators, and no pharmaceutical or device company took any part in the design or process of this study. In accordance with institutional policies, every patient gave written informed consent for TAVI and the use of the anonymous clinical, procedural, and follow-up data for research in accordance with institutional review board approval. This study complied with the Declaration of Helsinki.
From May 2007 until February 2012, we enrolled 104 symptomatic patients with severe aortic stenosis and high or very high risk for surgery who were referred to our center for possible TAVI. Severe aortic valve stenosis was defined as an aortic valve area <1 cm 2 (0.6 cm 2 /m 2 ), a mean transvalvular gradient >40 mm Hg, or a peak transvalvular velocity ≥4 m/s. Symptomatic aortic stenosis was defined as having dyspnea of New York Heart Association class ≥II, angina, or exertional syncope without other conditions possible to explain these symptoms. Surgical (aortic valve replacement) or nonsurgical (TAVI or medical) treatment was based on extensive clinical evaluation of individual patients by cardiac surgeons, interventional cardiologists, and all involved physicians. After additional technical evaluation (invasive evaluation, multimodality aortic root imaging), every patient was discussed by the multidisciplinary heart team, which finally proposed a preferred treatment strategy. The eventual presence of intracardiac thrombi was initially considered a contraindication for aortic valve replacement and TAVI, followed by an intensified antithrombotic strategy and reevaluation by TEE.
Transthoracic echocardiographic parameters assessed were left ventricular systolic function (normal: left ventricular ejection fraction [LVEF] >50%; impaired: LVEF 35% to 50%; severely depressed: LVEF <35%), degree of diastolic dysfunction (when atrial fibrillation was present, E/E′ ratio >11, deceleration time <150 ms, and isovolumetric relaxation time <65 ms were used to classify a patient as having severe [restrictive] diastolic dysfunction), left atrial size at end-systole (M-mode echocardiography in the parasternal long-axis view; normal value <40 mm), calculated aortic valve area and mean transvalvular gradient, and the severity of mitral regurgitation (grades 0 to 4) using color flow mapping. Transesophageal echocardiographic parameters assessed were the presence of intracardiac thrombus and the presence and degree of SEC, with a focus on the left atrium and LAA. No SEC was scored grade 0, localized SEC in the left atrium and LAA as grade 1, and dense SEC in the left atrium and LAA or stasis of SEC in the LAA as grade 2. Grade 2 SEC was considered significant SEC, with a potential thromboembolic risk ( Figure 2 ). Estimating the degree and presence of SEC was done by 2 level III echocardiographers working independently. Systolic LAA velocity was assessed using pulsed Doppler imaging. A systolic velocity <40 cm/s was considered to indicate a hypocontractile LAA. The presence of paroxysmal or permanent atrial fibrillation was assessed by medical history, electrocardiography, ambulatory Holter monitoring, and continuous rhythm monitoring during hospitalization. All patient medical files were reviewed. Antithrombotic therapy of each patient was documented.
Logistic regression analysis was used to assess whether parameters were associated with the presence of intracardiac thrombus and/or grade 2 SEC. Selected clinical variables were entered as individual independent variables in the logistic regression analysis, with the presence of thrombus and/or grade 2 SEC as dependent variable. Significant factors were then entered in a multiple logistic regression to determine the independent contributions of the different factors to predict the presence of thrombus and/or grade 2 SEC. Odds ratios and corresponding 95% confidence intervals are reported. Significance was set at p <0.05.
Results
Baseline characteristics of the patients included in the study are listed in Table 1 and reflect an old population with severe aortic valve stenosis at (very) high risk for surgery. Thirty-eight of 104 patients (36%) had documented continuous (n = 31) or paroxysmal (n = 7) atrial fibrillation. However, 9 of these 38 patients were not treated with warfarin before the procedure, for unclear reasons. Finally, after evaluation by the heart team, 71 patients (68%) underwent TAVI, 17 patients (16%) were treated medically, and 16 patients (15%) underwent surgical aortic valve replacement.
| Characteristic | Value |
|---|---|
| Age (yrs) | 80.4 ± 7 |
| Men | 45 (43%) |
| Logistic EuroSCORE (%) | 24.2 ± 15 |
| Aortic valve area (cm 2 ) | 0.63 ± 0.15 |
| Mean gradient (mm Hg) | 42.1 ± 14.6 |
| Atrial fibrillation | 38 (36.5%) |
| LVEF (%) | |
| >50 | 60 (58%) |
| 35–50 | 33 (32%) |
| <35 | 11 (11%) |
| Left ventricular diastolic dysfunction | |
| Impaired relaxation | 27 (26%) |
| Pseudonormalization | 28 (27%) |
| Restrictive | 49 (47%) |
| Left atrial size (mm) | 50.6 ± 7 |
| Mitral regurgitation grade 3 or 4 | 30 (29%) |
| Antithrombotic therapy before the procedure | |
| No antithrombotic therapy | 13 (12%) |
| Aspirin monotherapy | 30 (29%) |
| Thienopyridine monotherapy | 8 (8%) |
| Aspirin plus thienopyridine | 21 (20%) |
| Warfarin | 32 (31%) |
In 11 of 104 patients (11%), intracardiac thrombi were detected by TEE ( Table 2 ). Ten patients had thrombi in the LAA, and in 1 patient, a left ventricular apical thrombus was present. In the remaining patients without intracardiac thrombi (93 of 104), dense SEC (defined as grade 2) was detected in 25 (24%), grade 1 SEC in 24 (23%), and no SEC in 44 (42%). Of the 11 patients with intracardiac thrombi on TEE, 7 were ultimately eligible for TAVI after anatomic assessment and evaluation by the heart team. Continuous sinus rhythm was present in 2 of these 7 patients, but warfarin therapy was initiated because of thrombus presence, followed by control TEE after ≥6 weeks. Because of subtherapeutic international normalized ratios in the past months, the other 5 patients were started on low–molecular weight heparin temporarily while warfarin therapy was intensified and followed by control TEE after ≥6 weeks. In case of persistent thrombus despite optimal anticoagulation, TAVI was not performed. The 4 patients with intracardiac thrombi but not eligible for TAVI were also treated with therapeutic warfarin therapy. Using this strategy, bleeding complications were documented in none of the 11 patients.
| Variable | Value |
|---|---|
| Intracardiac thrombus | 11 (11%) |
| LAA | 10 (10%) |
| Left ventricle | 1 (1%) |
| No intracardiac thrombus | 93 (89%) |
| SEC grade 0 | 44 (42%) |
| SEC grade 1 | 24 (23%) |
| SEC grade 2 | 25 (24%) |
| LAA systolic velocity (cm/s) | |
| Mean | 41.9 ± 17 |
| <40 | 37 (36%) |
The 30-day incidence of stroke and TIA, according to the Valve Academic Research Consortium definitions, in those patients who ultimately were accepted for TAVI was 1.4% (1 of 71 patients, ischemic stroke) and most probably related to periprocedural valve embolization in this patient. When combining the observed echocardiographic abnormalities (intracardiac thrombus and dense grade 2 SEC), a total of 36 (11 with intracardiac thrombi and 25 with significant grade 2 SEC) of 104 patients (35%) referred for potential TAVI had an intracardiac thrombotic and therefore potentially embolic state. In a univariate analysis, no relation between the presence of thrombus and/or grade 2 SEC and age (p = 0.228), severity of the aortic valve stenosis (p = 0.826), LVEF (p = 0.191), logistic European System for Cardiac Operative Risk Evaluation score (p = 0.170), or mitral regurgitation (p = 0.255) could be demonstrated ( Table 3 ). Only 25 of these 36 patients (69%) with thrombi or dense grade 2 SEC had continuous or paroxysmal atrial fibrillation (p <0.0001), and 11 of these 36 patients (31%) were in continuous sinus rhythm, without documented atrial fibrillation. Severe diastolic dysfunction was present in 26 of 36 patients (72%), and the presence of thrombus and/or dense grade 2 SEC was significantly more frequent in the presence of diastolic dysfunction (p = 0.0005). Enlarged left atrial size was significantly associated with the occurrence of dense grade 2 SEC and thrombus, with a mean left atrial size of 53.6 ± 7.6 mm compared with a mean size of 49.0 ± 6.9 mm in those without intracardiac thrombi or significant SEC (p = 0.0038).
| Parameter | No Dense SEC or Thrombus (n = 68) | Dense SEC or Thrombus (n = 36) | p Value |
|---|---|---|---|
| Age (yrs) | 81.1 ± 5.9 | 79.1 ± 7.7 | 0.228 |
| Logistic EuroSCORE (%) | 22.7 ± 14 | 27.3 ± 17 | 0.170 |
| Mean gradient (mm Hg) | 41.9 ± 13.7 | 42.4 ± 16.3 | 0.826 |
| Mitral regurgitation grade 3 or 4 | 16 (23%) | 14 (39%) | 0.255 |
| LVEF <35% | 5 (7%) | 6 (17%) | 0.191 |
| Atrial fibrillation | 13 (19%) | 25 (69%) | <0.0001 |
| Severe diastolic dysfunction | 23 (34%) | 26 (72%) | 0.0005 |
| Left atrial size (mm) | 49.0 ± 6.9 | 53.6 ± 7.3 | 0.0038 |
| Warfarin therapy | 12 (18%) | 20 (56%) | 0.0002 |
| LAA systolic velocity (cm/s) | 48.3 ± 15.3 | 29.3 ± 12.8 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


