INDICATIONS/CONTRAINDICATIONS
Transcervical extended mediastinal lymphadenectomy (TEMLA) was developed to improve a diagnostic yield of staging of the mediastinal nodes for nonsmall cell lung cancer (NSCLC).1,2 TEMLA is performed in patients with pathologically proven operable NSCLC in whom the results of endobronchial ultrasonography with transbronchial fine needle biopsy (EBUS/TBNA) and endoesophageal ultrasonography and fine needle aspiration (EUS/FNA) were negative, regardless of the results of computed tomography of the chest (chest CT) and positron emission tomography combined with CT (PET/CT). In such patients TEMLA is an alternative for a mediastinoscopy, regarded as a gold standard of the mediastinal staging according to the ESTS guidelines.3
The second aim of TEMLA is a possible improvement of results of surgical treatment of NSCLC due to the bilateral extensive lymphadenectomy.
TEMLA is applicable also for removal of the metastatic nodes of the other malignancies such as the thyroid cancer.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
No special preparations for TEMLA are necessary except the standard preparation for general anesthesia.

Figure 5.1 The Rochard frame. (Aesculap-Chifa, Nowy Tomysl, Poland)
 SURGERY
SURGERY
Positioning of a Patient
TEMLA is performed in a patient in a supine position with the role placed under the upper back area, the same for the standard mediastinoscopy. The modified Rochard frame (Aesculap-Chifa, Nowy Tomysl, Poland) is used for elevation of the sternum (Fig. 5.1).
Surgical Technique of TEMLA
The operation starts from the 5- to 8-cm collar incision in the neck.
Subplatysmal flaps are widely dissected for better exposure of the mediastinum during the procedure. Visualization of both laryngeal recurrent nerves is obligatory in every case.
The detailed technique of visualization of the laryngeal recurrent nerves was described elsewhere.4 In brief, visualization of the right laryngeal recurrent nerve is started first. The carotid sheath of the right common carotid artery is divided with scissors, reaching the clean wall of the artery. The thyroid gland, the trachea, and the thymus gland are retracted to the left side with fingers and the right common carotid artery is retracted to the right side. Due to division of the deep fascial layers the right paratracheal space is easily accessible. Using blunt dissection with a peanut sponge the right laryngeal recurrent nerve is almost instantly visible. It runs from the point of division of the innominate artery toward the larynx. The deepest fascial layer covering the nerve is preserved, so the nerve is visualized, but not dissected; therefore, the risk of injury to the nerve is minimalized.
Visualization of the left laryngeal recurrent nerve is started after the right upper pole of the thymus gland is dissected free, grasped with a clamp, and retracted to the left side. The carotid sheath of the left common carotid artery is divided with scissors, the same as on the right side. The left common carotid artery is retracted to the left side and the trachea is retracted with the fingers to the right side. Using blunt dissection with the peanut sponge, the left laryngeal nerve is easily shown, running parallelly to the trachea in the tracheoesophageal groove (Fig. 5.2).
The left recurrent nerve is especially endangered during the procedure, so it must be dissected very delicately and carefully protected from injury. Circumferential dissection of the nerve is not advisable, in our opinion it increases the risk of injury to the nerve.
The central step of the presented technique is the division of the deep cervical fascial layers covering and obscuring the laryngeal recurrent nerves. Preservation of the deepest layer of the fascia protects the nerves from injury. No anatomical variations of the lower portions of both nerves were noted in this series—the nerves were in exactly the same location in all patients.
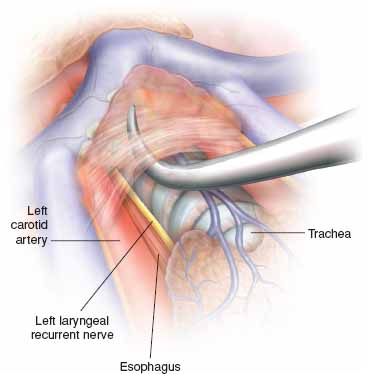
Figure 5.2 Dissection of the left laryngeal recurrent nerve. To expose the nerve, the vascularized fascial layers covering the nerve must be divided.
Both vagus nerves must also be found. The vagus nerve lies between the carotid arteries and internal jugular veins. The vagus nerves are the important landmarks for further dissection in the mediastinum.
Elevation of the sternal manubrium with a hook connected to the frame mounted on the operative table is a critically important part of the procedure (Rochard frame, Aesculap-Chifa, Nowy Tomysl, Poland) (Fig. 5.1). Elevation of the sternum widens access to the mediastinum from the neck and enables reaching the deeply located mediastinal structures.
During TEMLA all mediastinal nodal stations except for the pulmonary ligament nodes (station 9 according to the recent International Association for the Study of Lung Cancer (IASLC) map are sampled.5 Generally, most part of TEMLA is an open procedure, with exception of dissection of the subcarinal (station 7), periesophageal (station 8), and the left lower paratracheal (station 4L) nodes, which are dissected in the mediastinoscopy-assisted fashion with the aid of Linder–Dahan two-blade mediastinoscope (Richard Wolf, Knittlingen, Germany) (Fig. 5.3). The para-aortic, station 6 and aorta-pulmonary window, station 5 nodes are sometimes dissected with the aid of videothoracoscope introduced to the mediastinum through the operative wound. An attempt should be made to remove en-bloc the nodes with the surrounding fatty tissue. Only the left paratracheal (station 4L) nodes are removed individually, due to close proximity of the left recurrent nerve.
Bilateral supraclavicular lymphadenectomy and even deep cervical lymph node dissection is possible during TEMLA through the same incision.
The mediastinal dissection begins from removal of the highest mediastinal, station 1 lymph nodes lying above the left innominate vein. Resection of the upper poles of the thymus at the level of the left innominate vein improves access to the mediastinum (Fig. 5.4).6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


