INDICATIONS/CONTRAINDICATIONS
The omentum is used as a vascularized tissue flap for a variety of cardiothoracic surgical problems that are complicated by factors that impede wound healing, such as previous irradiation, established infection, or steroid use. Reinforcing anastomoses with well-vascularized tissue such as omentum provides delivery of oxygen, nutrients, and growth factors to facilitate healing. In addition, an omental flap transposition into an infected space can both obliterate the space and serve as a mechanism to deliver antibiotics to the region. An omental flap based upon a right gastroepiploic vascular pedicle is sufficiently long to reach any region of the chest, and any part of the airway including the cervical trachea. The bulk and pliability make the omentum particularly well suited for complete filling of irregular spaces. When used in the lower chest, its bulk is particularly evident and thus its ability to fill dead space is at a maximum; when the omentum is “unfolded” along its vascular arcades to reach higher in the chest, its bulk is attenuated and it is useful only in more focal applications.
Omental transposition can be used as a prophylactic aid for the healing or closure of airway and gastrointestinal anastomoses that are at high risk of failure, in the treatment of problems complicated by established infections including empyema, and less commonly to allow autologous tissue coverage following chest wall resection. Omental transposition achieves the goal of promoting safe healing of high-risk closures and anastomoses in the vast majority of difficult thoracic cases in which it is used for prophylactic or therapeutic purpose. Although there are no absolute contraindications to the use of an omental flap other than prior omentectomy, prior abdominal surgery may limit the availability of the omental flap and complicate its mobilization. Further, the use of the omentum in asthenic individuals will be limited by the possible minimal bulk of omental tissue.
 SURGERY
SURGERY
Omental Mobilization
Omental mobilization is usually performed through an upper midline incision extending from the tip of the xiphoid to the umbilicus although laparoscopic mobilization is also quite feasible. Detachment of the omentum only in the relatively avascular plane between the omentum and the transverse mesocolon, keeping both the right and left gastroepiploic arcades intact, and simply rotating the omentum up to the chest, will provide length sufficient to reach the level of the nipple in approximately two-thirds of patients. The partial rotation of the stomach that usually occurs as the omentum is rotated upward has been demonstrated to have no ill effect upon gastric emptying.
For more complete mobilization, the left gastroepiploic artery is divided at a point approximately two-thirds of the distance along the greater curve toward the spleen, at the point where the right gastroepiploic arcade fades. The gastroepiploic arch is then separated from the greater curve of the stomach by individual ligation and division of these gastric feeding vessels, taking great care to protect the origin and entire course of the right gastroepiploic artery (Fig. 51.1A). With the omentum pedicled in this way, enough length is gained to reach the base of the neck in 88% of patients. In the occasional case that it is necessary to gain further length, the arcade can be divided at one or more points (Fig. 51.1B), allowing the omentum to be “unfolded,” creating a long, thin pedicle. Transillumination of the arcades is very helpful in identifying the appropriate points of division. Further, because of the variability of the arcades, it is advisable to clamp the targeted arcades for a few minutes with noncrushing bulldog clamps and assure the absence of distal ischemia before committing to dividing them.
Routes of Transposition
The routes of transposition of the omentum into the chest are most commonly through (1) a substernal tunnel created immediately behind the retrosternal fascia then out through the mediastinal pleura, or (2) via an incision made in the diaphragm anteriorly near the costal attachments (Fig. 51.2A). If it is decided to use the omentum in a patient requiring a thoracotomy, it may be preferable (particularly in an infected chest) to first mobilize the omentum through the abdomen with the patient supine and to place the omentum in a substernal pocket that is created from within the abdomen in the same plane that one would find a Morgagni hernia. Following closure of the laparotomy, the patient is positioned for thoracotomy at which time the mediastinal pleura is opened and the omentum drawn fully into the hemithorax (Fig. 51.2B).
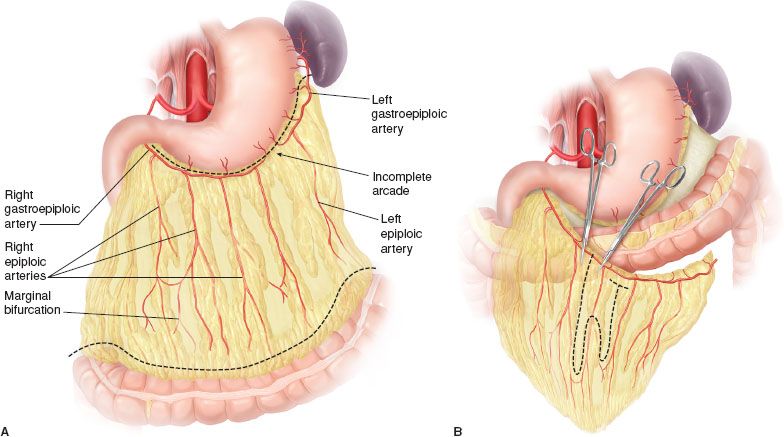
Figure 51.1 A: Anatomy of the omentum. Dashed lines represent line of division of the omentum from the stomach and from the transverse colon. Note that great care is taken to identify and preserve the right gastroepiploic artery, the primary blood supply of this flap. B: If further lengthening of the flap is needed, the arcade can be divided at one or more points to produce a longer pedicle. If this is necessary, vascular clamps are first placed at the sites of potential transection and the distal omentum is examined for viability before vascular division.
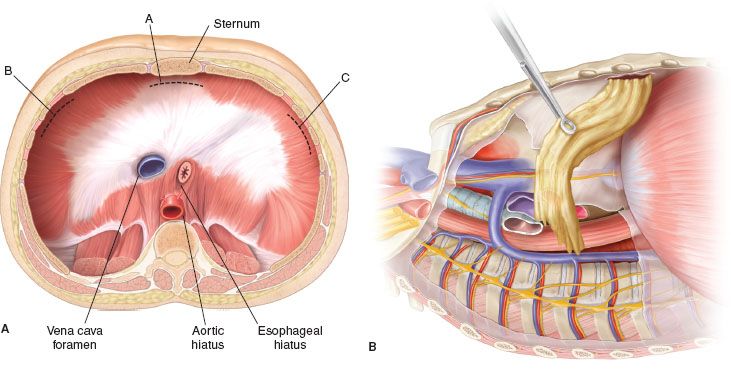
Figure 51.2 A: Diaphragmatic apertures for transposition of the omentum. The opening for substernal transfer is shown in the retrosternal position, and the lateral incisions indicate the region for anterolateral passage into the hemithorax. B: Following placement in a retrosternal pocket during the abdominal portion of this procedure, the mediastinal pleura is later divided inferiorly and the omentum is retrieved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


