Figure 28.1
The operation starts with a 5- to 8-cm collar incision in the neck. The subplatysmal flaps are widely dissected, and the muscles and vascular structures are liberated widely for better exposure during the procedure. In every case, the surgeon must be able to visualize both the right (R) and left (L) recurrent laryngeal nerves (RLNs; Zieliński et al. 2005). The left recurrent nerve is especially endangered during the procedure, so it must be dissected very delicately and protected from injury. Circumferential dissection of the nerve is not advisable. Preservation of the last layer of fascia covering the nerve is preferable. Both vagus nerves also must be located. The right vagus nerve lies between the right carotid artery and right internal jugular vein; the position of the left vagus nerve is similar. The vagus nerves are important landmarks for further dissection in the mediastinum. The mediastinal dissection begins with removal of the highest mediastinal (station 1) lymph nodes lying above the left innominate vein. Resection of the upper poles of the thymus at the level of the left innominate vein improves access to the mediastinum. SVC, superior vena cava (Adapted from Zieliński et al. (2006))

Figure 28.2
The next step is dissection of the right paratracheal space, which proceeds along the posterior wall of the superior vena cava until the azygos vein is visible. The right upper paratracheal (station 2R) nodes located above the apex of the aortic arch and below the left innominate vein are dissected and removed. The lower paratracheal (station 4R) nodes are dissected from the trachea, right main bronchus, superior vena cava, azygos vein, ascending aorta, and right mediastinal pleura. Very occasionally, retrotracheal (station 3P) nodes are found and removed; we have never found any metastatic lymph nodes in this station. For right-sided tumors, the next step is dissection of the prevascular (station 3A) nodes, located in front of the superior vena cava, to the right of the ascending aorta. This station is never involved in left-sided tumors. In my opinion, dissection of the left paratracheal nodes is the most difficult and risky part of TEMLA, because these nodes lie close to the left recurrent nerve. Generally, the left upper paratracheal (station 2L) nodes lie in front of the nerve and the left lower paratracheal (station 4L) nodes lie behind it. During dissection of the subcarinal (station 7) nodes, the fascial layer covering the nodes must be divided. Usually, a prominent bronchial artery crossing the operating field must be clipped and divided. The subcarinal nodes must be dissected from the trachea, main bronchi, esophagus, and main pulmonary arteries (Adapted from Zieliński et al. (2006))
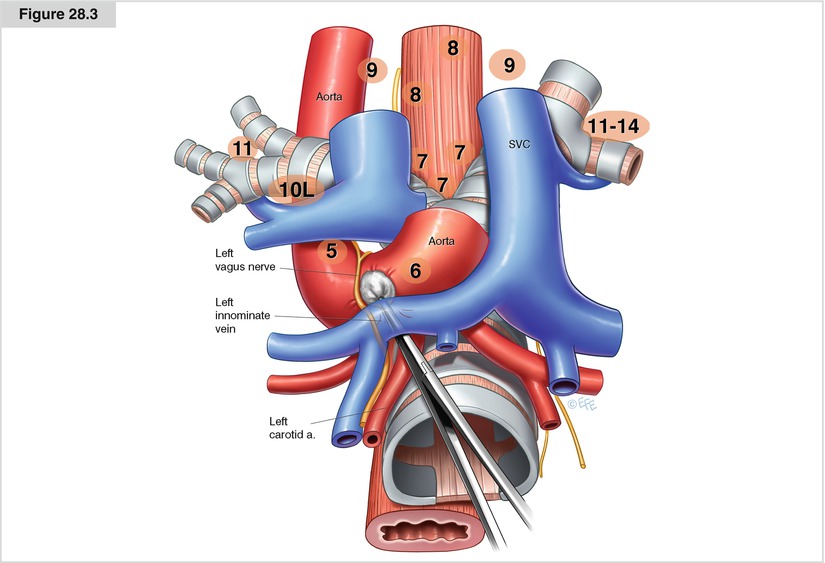
Figure 28.3




After dissection of the paratracheal spaces, the tracheal bifurcation, both main bronchi, both pulmonary arteries, the pericardium covering the left atrium, the right superior pulmonary vein, and the right upper lobe bronchus are clearly visible. In some—but not all—patients, the periesophageal (station 8) nodes are found and removed. Station 4L nodes are dissected with mediastinoscopic assistance after dissection of station 7 and 8 nodes. The entrance to the aortopulmonary window containing stations 6 and 5 lies between the left innominate vein and the left carotid artery. The left vagus nerve is a landmark for the dissection. Division of the fascial layer between the left carotid artery and left innominate vein facilitates entry to the aortopulmonary window. First, the adipose tissue is dissected with a peanut sponge from the wall of the ascending aorta down to the level of the left pulmonary artery. Medial retraction of the ascending aorta is a safe maneuver facilitating access to the aortopulmonary window. In some patients, complete mobilization of the left innominate vein is necessary to obtain good access to the para-aortic (station 6) nodes above the vein. All fatty tissue is removed from the aortopulmonary window space. Any blood vessels crossing the space are clipped and divided. Dissection proceeds along the left vagus nerve. The fatty tissue is then dissected from the left mediastinal pleura until the clear pleura and the underlying left lung are seen clearly (Adapted from Zieliński et al. (2006))
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


