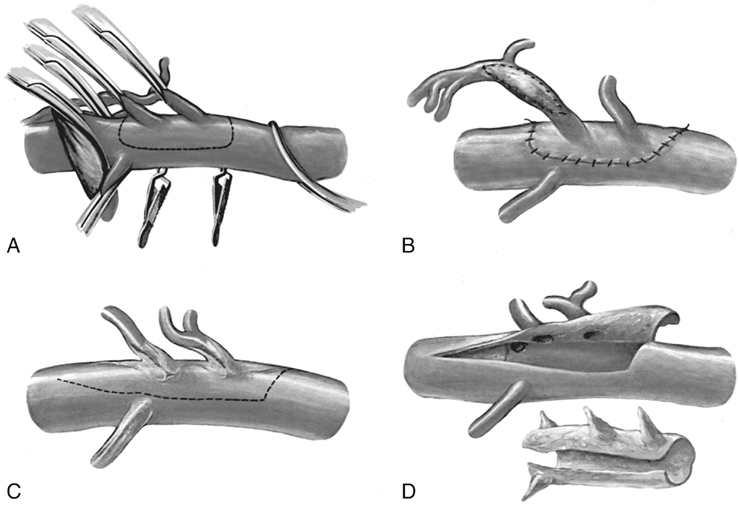
In parallel to the development of these techniques, Stoney, Ehrenfeld, and Wylie developed the alternative approach of transaortic mesenteric artery endarterectomy. This technique evolved from their experience in transaortic renal endarterectomy and was facilitated by development of the thoracoretroperitoneal aortic exposure. Transaortic mesenteric artery endarterectomy was accomplished through a trapdoor aortotomy and eversion endarterectomy of the mesenteric vessels (Figures 1 and 2). This technique was subsequently modified to avoid the complications of the thoracic incision by performing a medial visceral rotation to expose the midaorta through an abdominal incision.
Transaortic Splanchnic Endarterectomy for Chronic Mesenteric Ischemia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



