Fig. 8.1
The midline incision from manubrium to epigastrium. Here, the pectoral muscles are stripped back allowing for bilateral parasternal and subperichondrial resection of the deformed costal cartilages [2]
Fig. 8.2
How the surgeon gains access to the xiphoid, following division of the xiphisternal joint [2]
Fig. 8.3
Illustrates the resection of costal cartilages and intercostal bundles on both sides allowing the sternum to be freed from its lower end. A transverse osteotomy is performed [2]
Modification of Ravitch
Surgical repair of pectus excavatum relies on the corrected position of the sternum being maintained through the use of a sheet of synthetic mesh. Robicsek, 1978 presented a modification of the Ravitch procedure. This technique uses placement of Marlex mesh behind the sternum. The edge of the Marlex mesh is sutured to the peripheral stump of the resected ribs [3–5].
Following detachment of the xiphisternum, all loose mediastinal tissue is removed from the posterior sternum and the right pleural cavity drained with a chest tube, assuring optimal wound healing. The lower sternal end is bent forwards, breaking the posterior lamina at the transverse osteotomy. The Marlex mesh is spread tightly posterior to the sternum and has lateral attachments to the remaining costal cartilages on their anterior side. The corrected position of the sternum is now maintained and secured with the xiphoid process loosely attached to the lower end of mesh [3–5].
Comparative Studies
Recurrent pectus excavatum is experienced in a range of 2–37 % of patients having undergone corrective surgery for pectus excavatum. Common causes of recurrence include: asymmetric PE, perichondrium cartilage damage, limited space following retrosternal dissection, infection, improper fixation and early removal retrosternal plate [6]. The Ravitch procedure has few, yet potentially serious, complications. One of these is phrenic nerve injury. If there is laceration of the phrenic nerve, the patient has trouble breathing and suffers considerably more pain. Breathing regulation is altered. Phrenic nerve injury can be caused by direct trauma and 10 % of cases of phrenic nerve damage are caused by operative trauma. When diaphragm paralysis occurs, the patient may suffer type 2 respiratory failure and require mechanical assistance.
Complication rates between the Ravitch and the Nuss procedure are similar. Length of hospital stay or time to ambulation post-surgical procedure is also similar amongst the two groups and differs only minimally. The rate of reoperation due to bar movement and migration from site of placement was higher in the Nuss group. This is the main factor causing persistent deformation and worsening long term outcomes. Postoperative pneumothorax and hemothorax were also higher in the Nuss group, whereas duration of surgery was longer in the Ravitch procedure. Patient satisfaction is relatively high in both surgical procedures [1, 7, 8].
In addition, a modification of the Nuss procedure can be used in the corrective surgery of pectus carinatum. Two stabilisers are used to apply force to the sternum to depress the elevation and allow for fixation to the ribs on either side. This method is minimally invasive and does not require thoracoscopy (Fig. 8.6, Tables 8.1 and 8.2) [9].
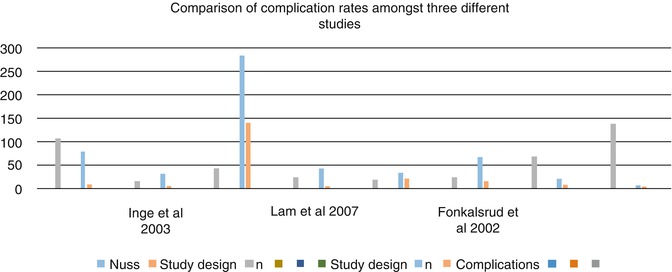
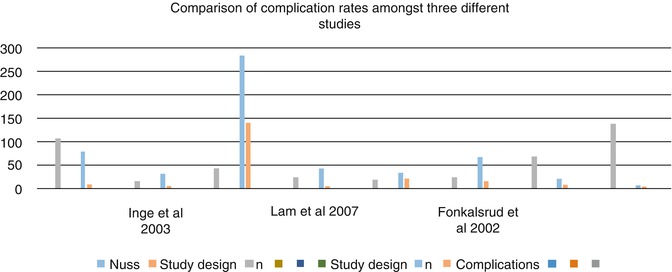
Fig. 8.6
Nuss procedure can be used in the corrective surgery of pectus carinatum. Two stabilisers are used to apply force to the sternum to depress the elevation and allow for fixation to the ribs on either side. This method is minimally invasive and does not require thoracoscopy (Adapted from Nasr et al. [1])
Table 8.1
Nuss procedure
Jo et al. [10] | Inge et al. [11] | Lam et al. [12] | Fonkalsrud et al. [13] | |||||
|---|---|---|---|---|---|---|---|---|
Nuss | Ravitch | Nuss | Ravitch | Nuss | Ravitch | Nuss | Ravitch | |
Study design | Retrospective | Retrospective | Retrospective | Retrospective | ||||
n | 107 | 16 | 43 | 25 | 19 | 24 | 68 | 139 |
Complications | 8 | 3 | 6 | 1 | 0 | 13 | 24 | 6 |
Reoperation | 3 | 0 | 3 | 0 | 0 | 0 | 7 | 0 |
Duration of surgery (min) | 67.2 ± 33.1 | 196.9 ± 61 | 70 | 198 | 72.1 ± 19 | 84.1 ± 24.9 | 75 ± 21 | 212 ± 37.5 |
Length of hospital stay (d) | 8 ± 1.6 | 15.9 ± 2.3 | 2.4 | 4.4 | 4.5 ± 0.9 | 3.9 ± 0.7 | 6.5 ± 0.75 | 2.9 ± 0.75 |
Time to ambulation | 6.3 ± 0.9 | 12.9 ± 3.6 | – | – | 3.8 ± 1.1 | 2.7 ± 0.8
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||