Figure 6.1
(a) For the cervical approach, the patient commonly is intubated with a single-lumen tube under general anesthesia and is placed in a supine position with the neck hyperextended. A 4- to 5-cm wide transverse incision is made above the sternal notch; the access may be enlarged by a T-shaped extension into the sternal notch. The skin, subcutaneous fat, and platysma are elevated as one layer, and the flap is raised to the level of the suprahyoid region. The infrahyoid muscles are divided along the midline down to the sternum, and the pretracheal fascia is opened longitudinally. The trachea is dissected digitally down to the carinal level. If the innominate artery is within the surgical access, it has to be dissected and moved away from the anterior tracheal wall. (b) The anterior wall of the trachea is incised at a length of 3–4 cm longitudinally in the midline at the level of the laceration. The exact level can be determined intraoperatively under endoscopic control after withdrawal of the tracheal tube. If ventilation cannot be interrupted during the incision of the anterior tracheal wall, the tracheal tube must be placed with the cuff distal to the laceration to avoid carving into the tracheal cuff
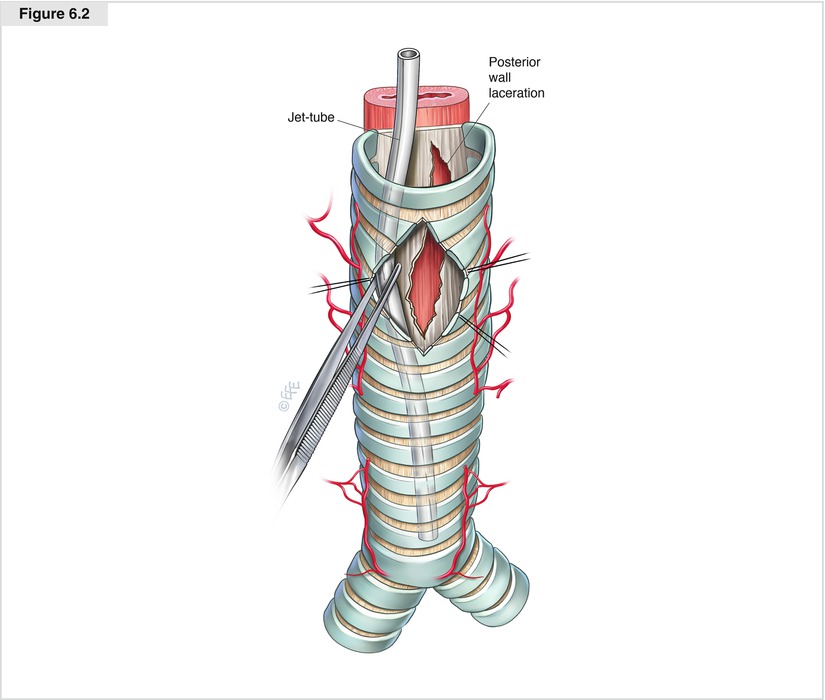
Figure 6.2
After incision of the anterior tracheal wall, the tracheal tube is withdrawn to enable access to the posterior tracheal wall; a Jet tube for high-frequency jet ventilation is introduced via the single-lumen tube, crossing the injured part of the trachea, and is placed into the distal part of the trachea. If the laceration reaches down to the tracheal bifurcation, the Jet tube is placed into a mainstem bronchus, or two Jet tubes may be placed in each mainstem bronchus. The Jet tube should be retained with forceps during the whole procedure. Subsequently, the tracheal laceration, particularly its depth, is examined to exclude accompanying injuries, such as those to the esophagus
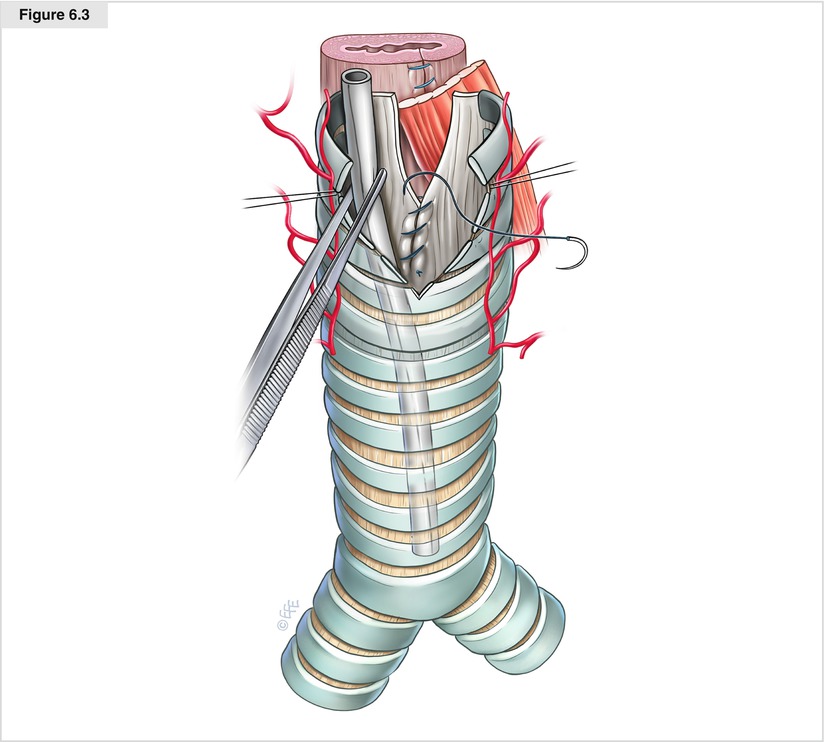
Figure 6.3
The tracheal laceration may be sewed with a running (4-0 resorbable monofilament) suture beginning at the distal bottom and running upward to the upper ending. If the laceration reaches down to the tracheal bifurcation, video-assisted thoracic surgical instruments and an additional light source may be helpful. The suture should include all layers of the posterior tracheal wall and render the margins of the laceration airproof. If there is an additional perforation of the anterior esophageal wall, it must be repaired separately with a running suture. A pedicular muscle flap should be interposed between the tracheal and esophageal sutures. During sewing of the trachea, the Jet tube is retained in the correct position in the distal trachea or mainstem bronchus to ensure sufficient intraoperative oxygenation of the patient
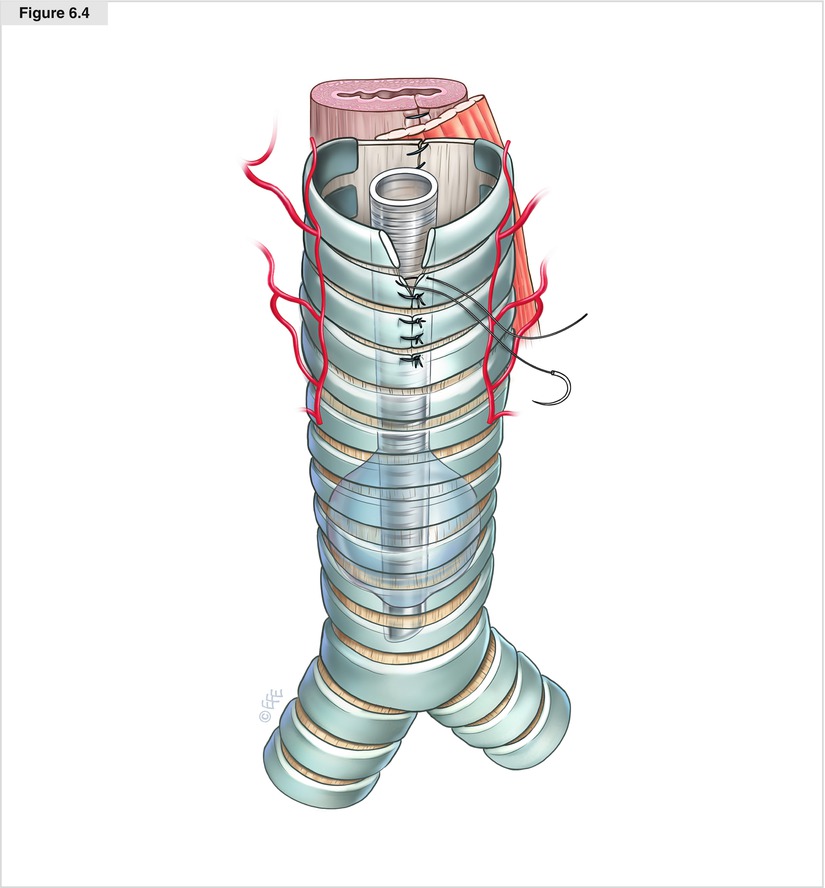
Figure 6.4
After suturing of the posterior tracheal wall is complete, the single-lumen tube is placed again with the cuff positioned distal to the laceration. The incision of the anterior tracheal wall is closed with interrupted sutures. The stitches are passed through both the intercartilaginous membranes and the cartilaginous rings—the edges of the suture should be joined together and should not overlap. The wound is closed in layers; a Redon drainage tube may be placed subcutaneously
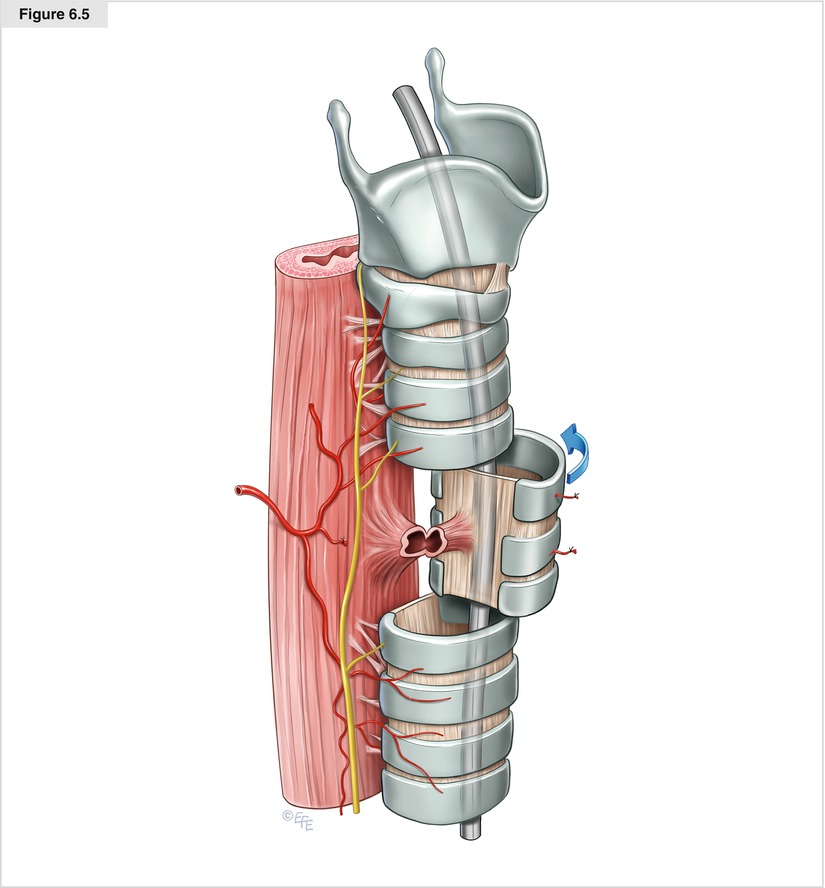
Figure 6.5




The surgical approach to a cervical fistula requiring tracheal resection is an anterior U-shaped cervical incision including an eventual tracheostomy stoma; for upper thoracic fistulae, the access can be enlarged by a T-shaped extension to the sternal notch. The skin, subcutaneous fat, and platysma are elevated as one layer, and the flap is raised to the level of the suprahyoid region. The sternohyoid muscles are divided in the midline, and the thyroid isthmus is divided and ligated to expose the anterior surface of the trachea. The trachea is freed circumferentially only above and below the site of the fistula, and care must be taken to maintain the dissection as close to the outer tracheal surface as possible to avoid injury to both recurrent laryngeal nerves and to preserve the lateral blood supply to the uninvolved parts of the trachea. The trachea then is divided in a healthy plane above and below the stenosis. Once the distal airway is divided, ventilation is obtained by a catheter for high-frequency jet ventilation into the distal tracheal airway; the catheter is introduced via the single-lumen tube, which has been withdrawn by the anesthetist
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


