Figure. 32.1
Minimally invasive thoracoscopic surgery using the three-armed da Vinci telemetric robotic system (Intuitive Surgical, Sunnyvale, CA). The procedure is performed under general anesthesia with single-lung ventilation. The patient is placed in the supine position on a vacuum mattress with the operating table tilted slightly to the patient’s right. The left arm is positioned below the table level with flexion at the elbow. The surgeon and assistant initially stand left of the patient. The operative field is always prepared and draped for conversion to a median sternotomy or other cervical approach or right-sided thoracoscopy, if necessary. The 12-mm trocar for the binocular camera is placed in the fourth intercostal space at the left anterior axillary line. A thoracoscopic 10-mm camera with a 30° optic is introduced to evaluate the operative field and to help position the other two 8-mm trocars. The cranial trocar is introduced in the third intercostal space anterior to the anterior axillary line; the caudal trocar is located in the fifth intercostal space between the anterior axillary and the midclavicular line. Thus, all three trocars are placed exactly along the submammary fold. The special da Vinci trocars are connected to the three robotic arms of the table cart. Harmonic shears (Ethicon Endo-Surgery, Cincinnati, OH) are placed in the upper trocar and precision bipolar forceps in the lower one. No auxiliary trocars are necessary
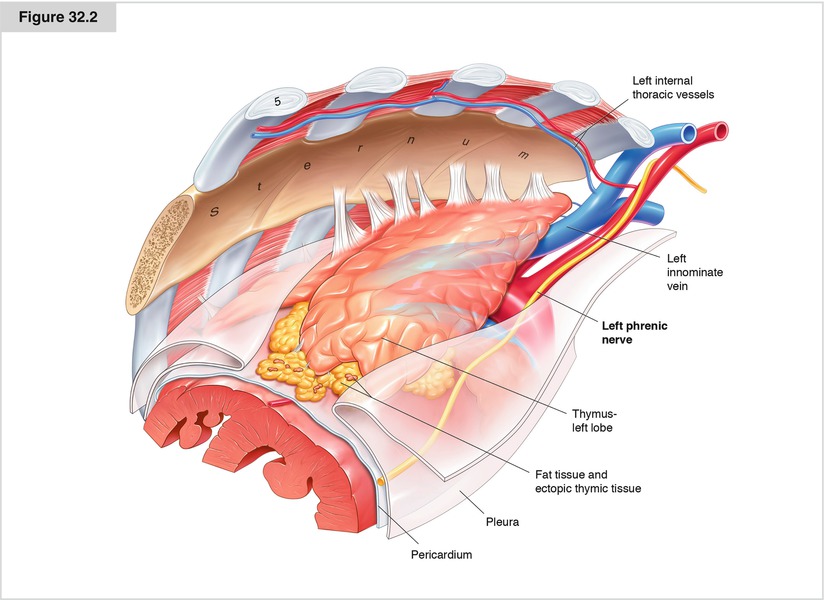
Figure. 32.2
The point of reference at the beginning of the dissection is the left phrenic nerve. The thymus gland may be partially visible depending on the amount of pericardial fatty tissue and the thymic histology. If there is a huge amount of fatty tissue, carbon dioxide may be applied initially. The dissection starts caudally in the middle of the pericardium along the left phrenic nerve. In younger, thinner patients, this area very often is completely free of fatty tissue, but in older, more obese patients, there is a lower fat district in the middle of the pericardium
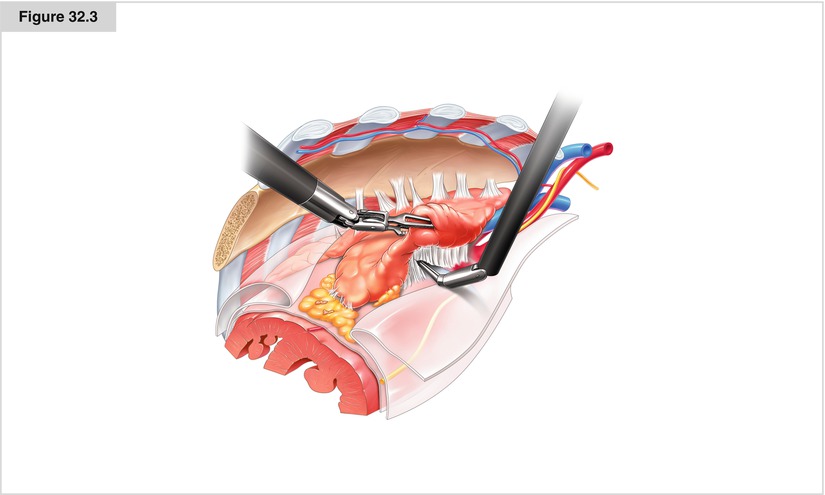
Figure. 32.3
The dissection is started along the left phrenic nerve. In some cases, the thymus gland extends below or above the phrenic nerve. In these cases, it is necessary to isolate the phrenic bundle and completely mobilize the tissue in the aortopulmonary window. Further dissection is done cranially along the phrenic nerve until the cervical pleura is identified and opened at the entrance to the innominate vein
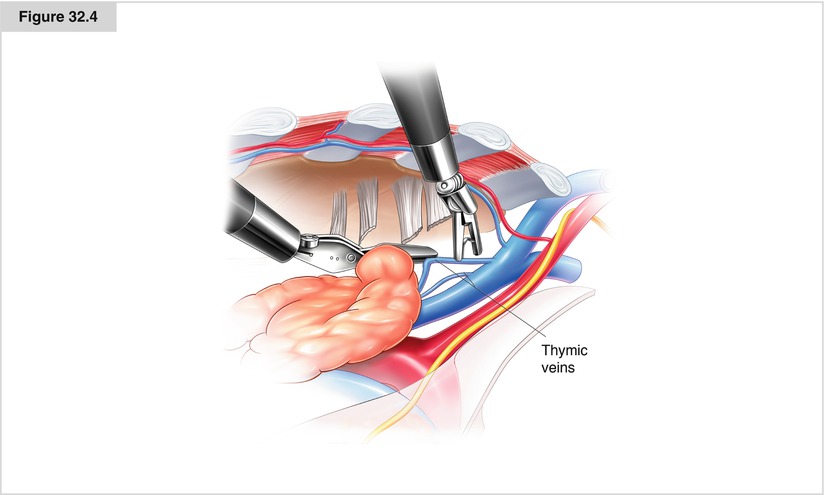
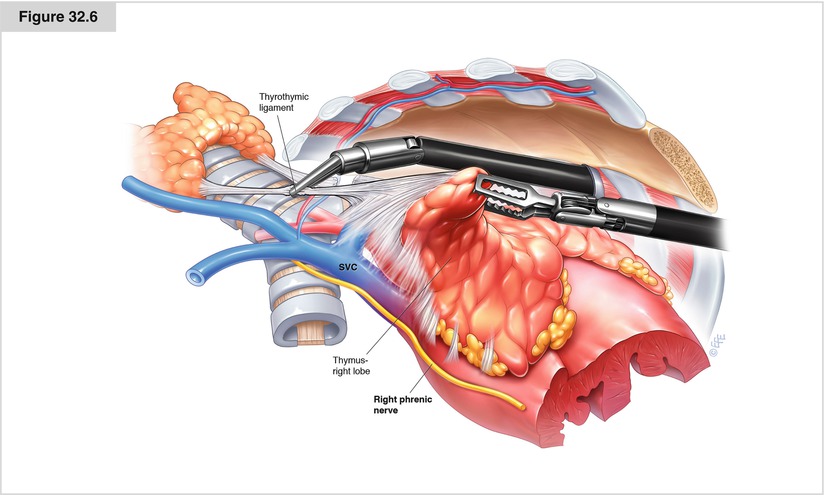
Figure. 32.4
Next, the retrosternal pleural incision is continued up to the jugular fold of the mediastinal pleura. To continue the preparation into the neck from behind the manubrium sterni, the mediastinal fold is incised. At this point, the anterior wall of the innominate vein is visible to the left of the phrenic nerve. Depending on the amount of fatty tissue in the anterior mediastinum, the vein may be located directly beneath the pleura or at a distance of more than 5 mm. Occasionally, a single central vessel, the so-called vein of Keynes, collects all the venous blood from the thymus gland for drainage into the innominate vein. In most cases, however, two to four thymic veins exist and must be dissected without injury to the innominate vein. The veins are divided between clip ligatures, although severing them with an ultrasonic scalpel also may be possible. Although rare, atypical locations of thymic veins must be considered
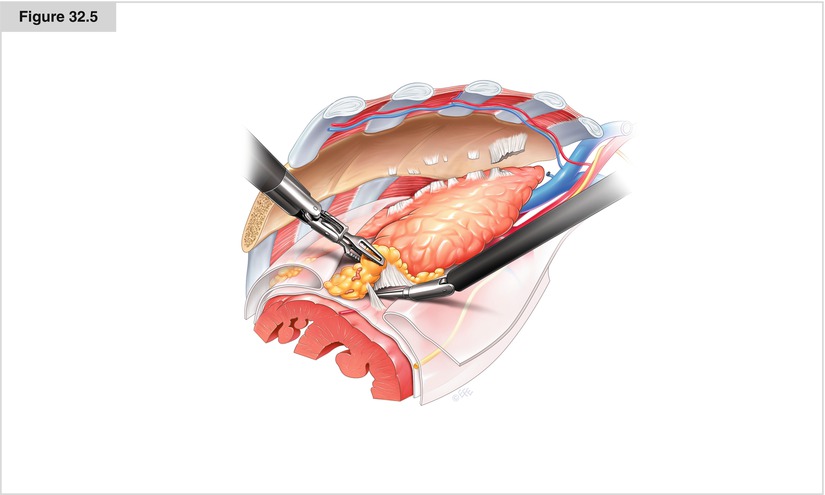
Figure. 32.5
The cervical pleural fold incision is extended to the median retrosternal line. The dissection is continued to the right side until it reaches the subxiphoid pleural fold. Beginning at the caudal pericardium, the tissue bloc is mobilized further on the pericardium. Depending on the patient’s age, constitution, histology, and immune suppression status before surgery, the various local findings will dictate whether to perform an almost complete blunt dissection or a very subtle ultrasonic dissection of small vessels from the pericardium. With gentle blunt dissection, the right lung is made visible and is covered only by the right pleura parietalis. Whenever possible, the right pleural cavity should stay closed during this stage of the operation, which will allow the operative field to be extended by carbon dioxide insufflation