Complication
Incidence (%)
Atrial arrhythmia
20.2
Reintubation
5.6
Pneumonia
4.6
Adult respiratory distress syndrome
3.1
Tracheostomy
2.5
Ventilator support >48 h
2.1
Sepsis
1.7
Reoperation for bleeding
1.5
Ventricular arrhythmia
1.0
Bronchopleural fistula
0.8
Pulmonary embolus
0.8
Myocardial infarction
0.8
Central neurologic event
0.6
Empyema
0.6
Independent risk factors for developing perioperative complications are age greater than 65 years, male sex, pneumonectomy for benign disease, and congestive heart failure. Current smoking, right-sided pneumonectomy, and neoadjuvant radiation therapy have been problems in some reports but were not significant using data from the STS general thoracic database. Unfortunately, outcomes based on pulmonary function were not predicted from this database because of missing spirometry data.
Pneumonectomy traditionally has been performed by thoracotomy, but minimally invasive approaches are gaining popularity at specialized centers and are discussed in Chap. 15. After adequate attainment of single-lung ventilation, the first step in any pneumonectomy is ensuring the feasibility of complete (R0) resection and the absence of occult metastatic disease in the ipsilateral chest. The pleura is opened to expose the hilar bronchovascular anatomy to confirm operability, and the need for intrapericardial vascular division is determined.
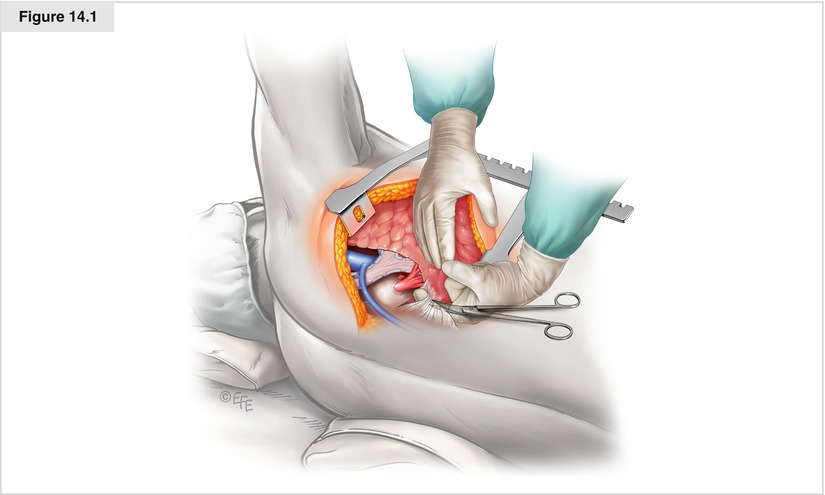
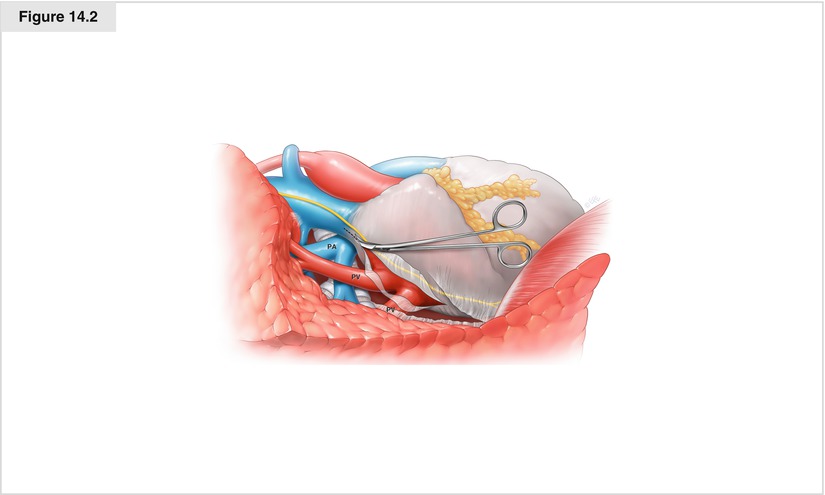
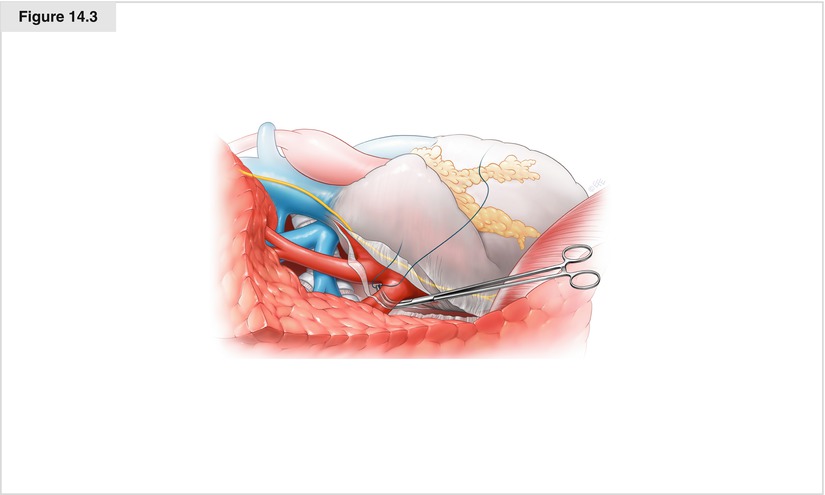
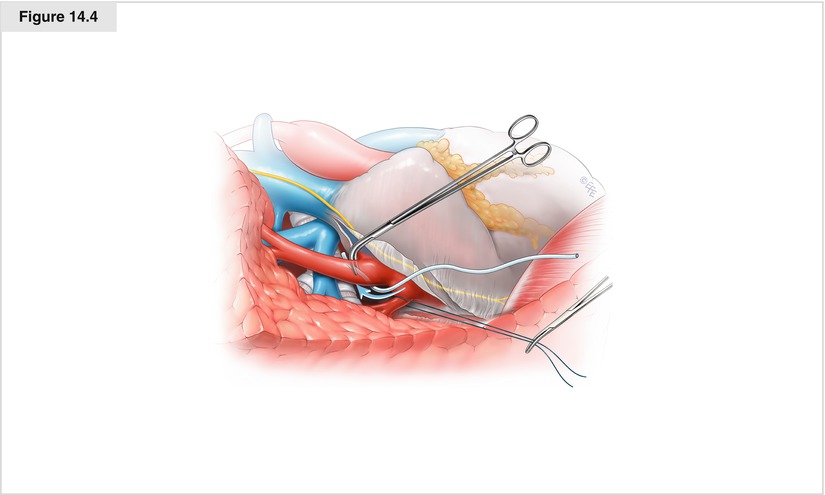
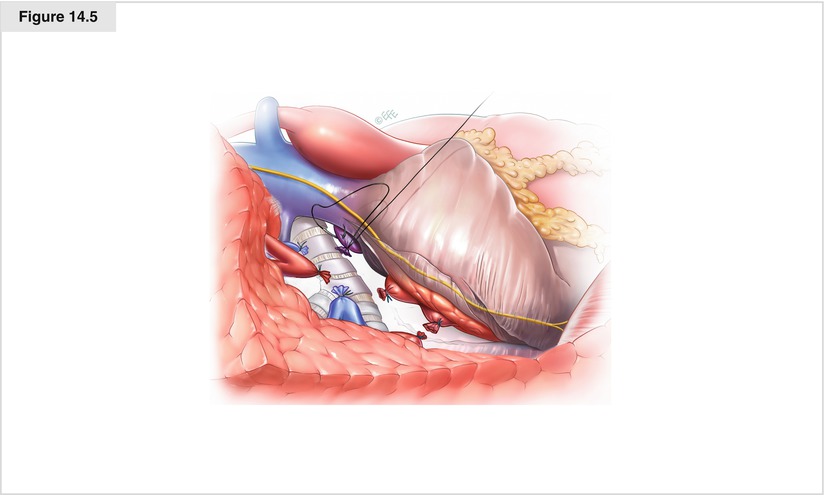
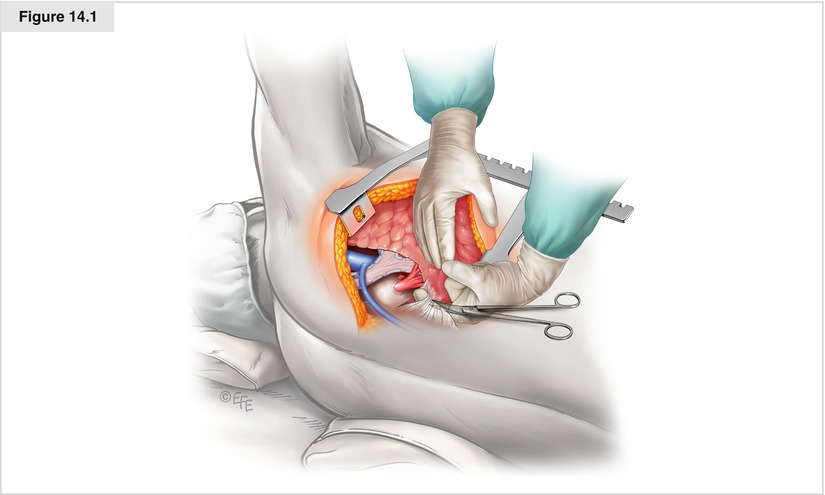
Figure 14.1
A muscle-sparing posterolateral thoracotomy is performed in the fifth intercostal space. Division or shingling of the posterior sixth rib allows optimal spreading of the ribs (see Chap. 2). The chest is explored thoroughly for metastatic disease and confirmation that hilar dissection is possible with grossly clear margins either within or outside the pericardium. The inferior pulmonary ligament is divided
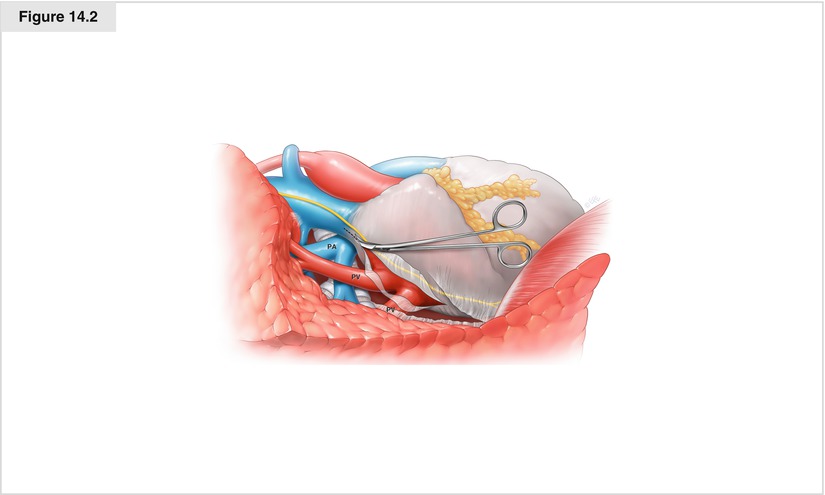
Figure 14.2
Any lymph nodes visualized are dissected and sent for pathologic analysis. If intrapericardial dissection is necessary, the pericardium is opened on the hilar side of the phrenic nerve and extended from the pericardial reflection from the inferior vein to the pericardial reflection at the superior portion of the pulmonary artery (PA). The inferior pulmonary vein (PV) is dissected circumferentially
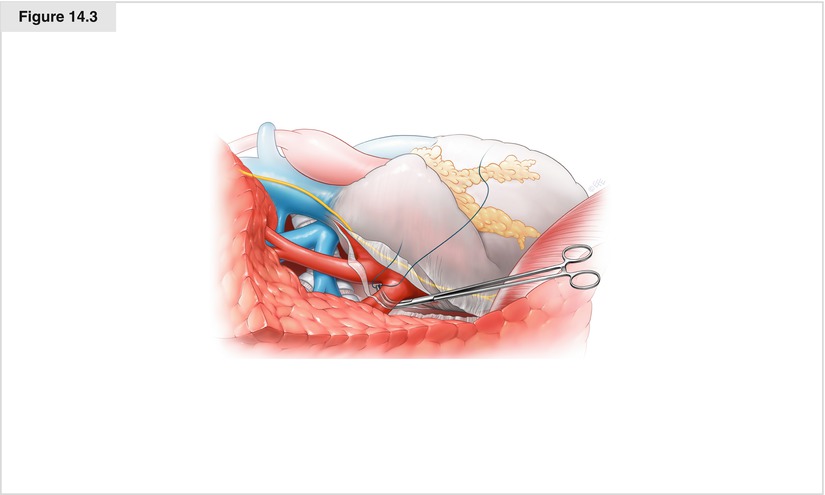
Figure 14.3
A vessel loop or tie may be passed if desired
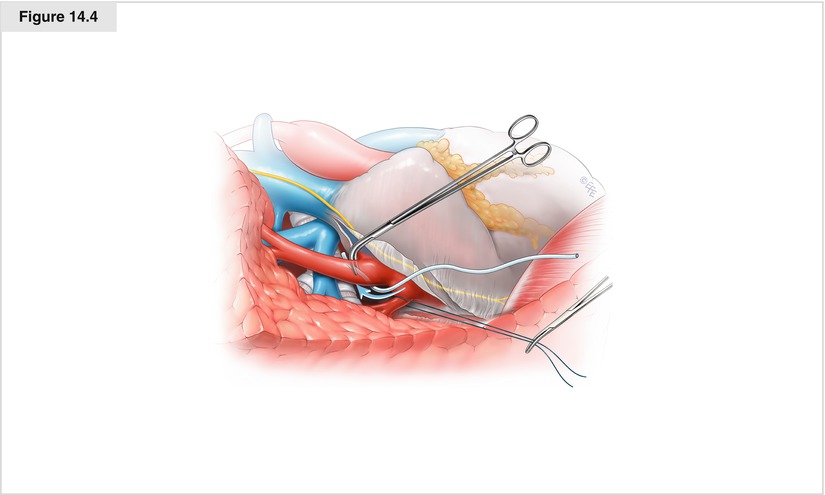
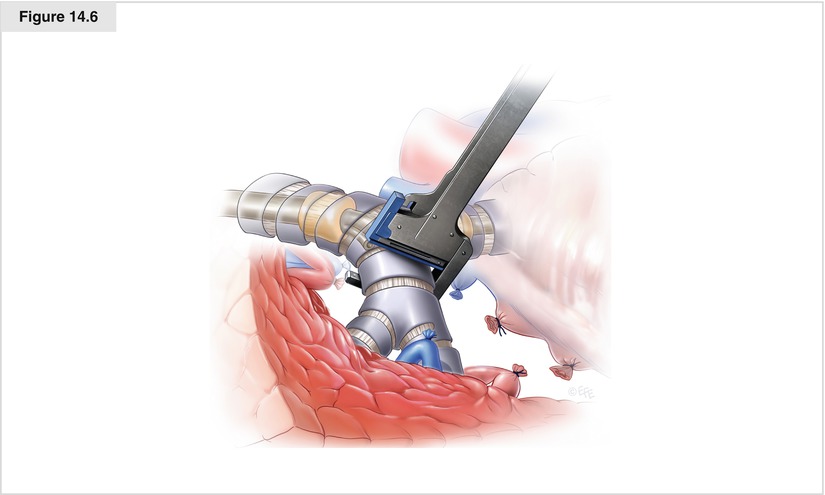
Figure 14.4
The superior pulmonary vein is dissected circumferentially, and a vessel loop is passed if desired to help facilitate ligation. The inferior and superior pulmonary veins are ligated and divided with either transfixing sutures and scissors or cutting staplers. Circumferential dissection of the main pulmonary artery is performed, and a vessel loop is passed twice to allow occlusion of the pulmonary artery
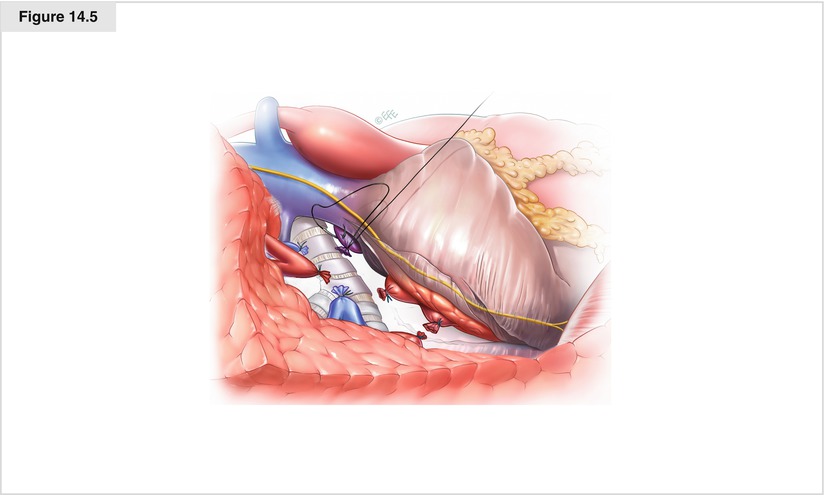
Figure 14.5
After the pulmonary artery is occluded for approximately 1 min, hemodynamic and respiratory stability are confirmed. The artery is then ligated and divided with a transfixing suture or vascular stapler