INDICATIONS/CONTRAINDICATIONS
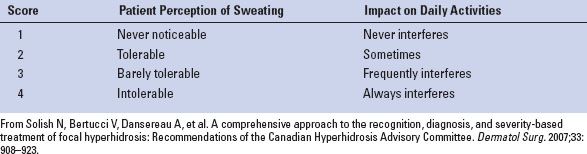
Assessment of hyperhidrosis severity is important for effective management. The Hyperhidrosis Disease Severity Scale (HDSS, Table 25.1) categorizes disease into “mild” (sweat that is not noticeable and does not interfere with daily activities), “moderate” (sweat is tolerable and sometimes interferes with daily activities), and “severe” (sweat is intolerable and interferes with daily activities). Patients who fall into the “severe” category often fail medical management.
While patients with severe palmar hyperhidrosis are likely to fail medical management, we feel that all patients should undergo a trail of medical therapy tailored to their specific symptoms. First-line treatment generally consists of topical therapy using antiperspirants and/or anticholinergic preparations. The most common, effective topical antiperspirants contain aluminum salts. We usually recommend that a 20% “prescription strength” aluminum salt antiperspirant be applied daily at bedtime to the affected areas. For many patients, a residual benefit lasts throughout the next day. Typical side effects include irritation or maceration of the skin, which is usually dose dependent. We also frequently recommend a compounded preparation of topical glycopyrrolate (2% to 4% w/w), as a cream, lotion, or alcoholic spray. This is typically applied up to three times per day and can be used in conjunction with an antiperspirant. Occasional systemic anticholinergic side effects are seen when large areas are treated aggressively.
As a next line of medical therapy, we typically prescribe an oral anticholinergic agent, such as oxybutynin, which is available in a long-acting formulation suitable for daily use. This class of medication is recommended with all of the caveats and precautions associated with any systemic anticholinergic therapy. Particular care is needed to educate patients about its potential effect of over-inhibiting perspiration, putting the patient at risk for heat stroke. It is best used in combination with topical therapies to maximize effect and minimize the dose-dependent side effects associated with any one particular drug.
TABLE 25.1 Hyperhidrosis Disease Severity Scale (HDSS)
For small areas of focal problematic hyperhidrosis, treatment with botulinum toxin injections is also an option. The drawback to this treatment modality is the need for repeated, often expensive, treatments. It is not practical for use on large areas.
Finally, for axillary hyperhidrosis only, the proprietary miraDry system is also of potential benefit. This treatment modality relies on the use of externally applied microwave energy to ablate the eccrine glands in the axillae. It is not currently approved for use outside the axillae.
We have found other treatments such as clonidine, beta-blockers, calcium channel blockers, benzodiazepines, and iontophoresis to be largely ineffective for most patients.
For patients who fail medical therapy, and who are principally bothered by palmar hyperhidrosis, we will offer a video-assisted thoracoscopic surgery (VATS) sympathectomy, ablating the T2-T3 ganglia. We will also offer this operation to patients with refractory axillary hyperhidrosis, with the understanding that the efficacy of this procedure is somewhat less in this subset of patients. It is imperative that all patients understand that some unpredictable degree of compensatory hyperhidrosis (usually below the T4 dermatomal level) is an expected result of this operation. It is incumbent upon the patient to make the final decision to accept this trade-off. In our experience, a small percentage of patients (<5%) regret having surgery due to excess compensatory hyperhidrosis, despite our best efforts to select and inform patients properly.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
There is much controversy over the appropriate level(s) and length of sympathectomy. As stated above, sympathectomies higher than the T2 level are often needed for reliable relief of craniofacial hyperhidrosis, and such sympathectomies carry a very high risk of inducing Horner syndrome. Palmer hyperhidrosis appears to be well controlled with ablations involving T2 and/or T3. Control of axillary hyperhidrosis typically requires a T3-T4 sympathectomy. There is also some evidence to suggest that shorter sympathectomies minimize compensatory hyperhidrosis, usually with some detriment to the primary efficacy of the operation.
In 2011, the International Society on Sympathetic Surgery (ISSS) and The Society of Thoracic Surgeons (STS) General Thoracic Task Force on Hyperhidrosis provided a consensus statement about the surgical treatment of hyperhidrosis. Among their recommendations was the use of a rib-oriented nomenclature, with “R” referring to rib, followed by the rib number and location of nerve division. In practice, the rib level is easier for the surgeon to identify than the sympathetic chain or ganglia, which does not, in reality, have the obvious stylized appearance presented in most anatomy texts.
Using this convention, our practice has focused on reliably treating patients whose primary complaint is palmar hyperhidrosis by means of a sympathectomy beginning on the middle of the second rib, and extending down to the top of the fourth rib, which corresponds roughly to a T2-T3 sympathectomy, allowing for individual anatomic variation. We have found that this approach produces nearly 100% complete and permanent control of palmar sweating, with no occurrences of Horner syndrome, and little (<5%) dissatisfaction due to excessive compensatory hyperhidrosis.
 SURGERY
SURGERY
Historically, upper thoracic sympathectomy was performed in an open fashion through posterior, supraclavicular, anterior thoracic, or transaxillary approaches. However, adequate exposure is often difficult via open approaches, and such cases were often accompanied by debilitating muscular pain/dysfunction, scarring, and increased risk of Horner syndrome particularly with the supraclavicular approach.
The advent of videothoracoscopy greatly facilitated the performance of a thoracic sympathectomy, by providing superior visualization and smaller incisions. Today, a bilateral VATS sympathectomy is typically a well-tolerated outpatient procedure that can be accomplished in under an hour.
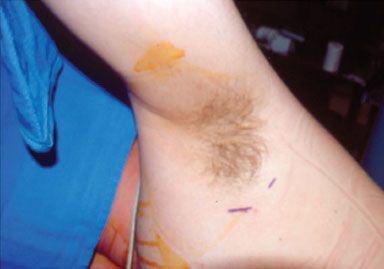
Figure 25.1 Left axillary exposure with markings for both 5-mm port sites.
Positioning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


