INDICATIONS
The best indication for an en bloc spondylectomy is the presence of a solitary well-demarcated tumor contained within the periosteal layer of a vertebral body, without extension to the epidural space or paravertebral structures. Such a strict requirement is relatively uncommon in clinical practice, thus limiting the application of this technique to special selected cases of primary spinal tumors, when the goal of surgery is cure. If these conditions are not met, the goal is immediately downgraded to long-term control of the disease, which is acceptable in cases of primary vertebral tumors with partial response to adjuvant treatment and have no gross extravertebral extension or selected cases of solitary spinal metastasis with controlled systemic disease.
We believe this technique should not be applied in cases where a gross total resection is not feasible, or when long-term local control of disease does not affect functional status or survival.
Surgical Staging and Planning
Meticulous preoperative imaging evaluation of the chest, abdomen, and pelvis is required to ascertain that disease is restricted to the vertebral body. Usually MRI with contrast and CT scans are both utilized for this purpose. A CT scan is useful for studying the anatomy of the adjacent pedicles and for planning the extension of the spinal stabilization. An extensive biomechanical analysis is out of the scope of this review, but in general for the nonmobile thoracic spine (T3 to T10), pedicle screw stabilization of two levels above and below the resected level is adequate. When the procedure is performed in junctional levels (T1 to T2 and T11 to T12), we recommend pedicle screw stabilization at least three levels above and below the resected vertebral body.
The thecal sac is surrounded by a bony ring composed by the vertebral body, pedicles, and a posterior arch formed by the laminas and spinous process. To pull the vertebral body away from the contents of the thecal sac, the posterior arch needs to be disconnected from the vertebral body. This requires at least two cuts, which needs to be performed in a bone without tumor. The most useful surgical classification for planning feasibility of an en bloc resection is the Weinstein–Boriani–Biagini classification, commonly referred as the WBB staging. This classification subdivides the vertebra in 12 radiating zones numbered 1 to 12 clockwise and 5 concentric layers labeled A to E from prevertebral to epidural involvement. Ideally for an en bloc resection tumor needs to spare one pedicle (zones 3 to 9, or 4 to 10), and be contained within the vertebral body (layers B, C, and D).
 SURGERY
SURGERY
Preparation and Positioning
The procedure is performed from a single posterior midline exposure; it is our routine to have motorization of somatosensory (SSEPs) and motor (MEPs) evoked potentials. We do not monitor electromyography, so the patient can receive paralytics throughout the case. We recommend 10 mg of dexamethasone to be given prior to the skin incision; however, the protective role of high doses of steroids is uncertain. The patient is positioned prone with arms tucked to the side or with arms abducted with the elbows flexed at 90 degrees “superman position,” depending on the level to be removed and the utilization of image guidance or fluoroscopy. Either a Jackson table, or gel rolls in the chest and iliac crest region provide adequate body support and decompression of the abdomen to avoid excessive epidural congestion. It is our preference to place patients in the Mayfield head holder to avoid pressure on the eyes and face during the procedure.
One of the most important factors in such procedure is localization of the accurate level. Since the tumor is contained within normal bony edges, all vertebral bodies will have a relatively normal appearance in the intraoperative fluoroscopy images. We usually use live fluoroscopy in anteroposterior and lateral projections to count pedicles from the bottom (sacrum) to top (level of interest). We always double check the count since performing resection at the wrong level is an unacceptable mistake. Once the level of interest is identified, the skin exposure is marked on the midline, extending at least two spinous processes above and below the tumor.
Exposure
A midline approach is performed and subperiosteal dissection of the paraspinal musculature with monopolar cautery exposes the spinous processes, laminas, and transverse process of at least two levels above and below the resection. Both ribs attached to the pedicle of the level of interest and the level below has to be exposed 10 to 12 cm laterally in the paraspinal region. This additional exposure is needed for resection of the rib heads to allow adequate access to the intervertebral discs and pleural space above and below the tumor. An Allis clamp is placed on the transverse process of the level planned to be resected and the level is again confirmed with AP and lateral fluoroscopic images. If the surgeon is using image guidance, the parameters for the navigation require an intact lamina and spinous process for registration; therefore, this step is performed prior to the laminectomy. We recommend placing the spinal instrumentation at this stage.
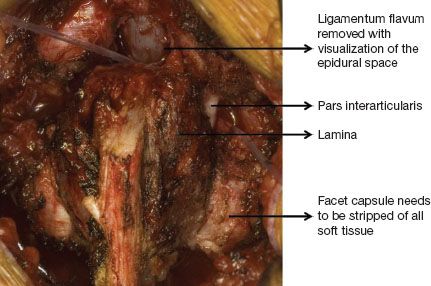
Figure 31.1 En bloc removal of the posterior elements. The ligamentum flavum above and below the lamina is removed exposing the epidural space. All soft tissues under the pars interarticularis are dissected and a plastic malleable tube is passed under the lamina from rostral to cudal and medial to lateral. Next a thread wire saw is used to cut the pars with reciprocating movements.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


