11 Thoracic aorta
The prevalence of aortic pathology is steadily increasing as a result of:
AORTIC DISSECTION
The limitations and pitfalls of TEE relate to:
Pitfalls when diagnosing dissection
Specificity of the echocardiographic signs
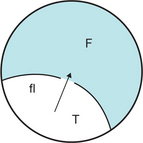
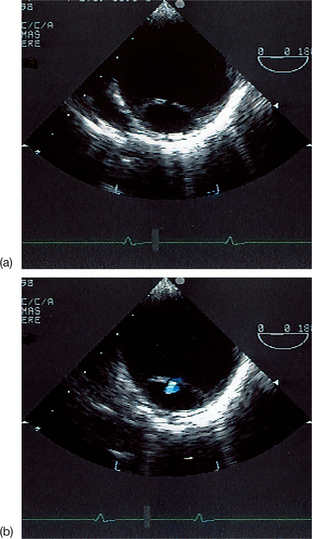
The echocardiographic diagnosis of aortic dissection is based on the visualization of the mobile intimal flap, floating between the true and false lumen (Figs 11.1 and 11.2).
Overdiagnosis of aortic dissection
False-positive diagnoses of aortic dissection (Box 11.1) are dominated by:
Box 11.1 Causes of false-positive diagnosis of aortic dissection when using TEE
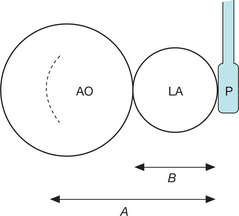
Linear artefacts, which are located principally on the ascending aorta, are frequently observed in monoplanar TEE. The use of multiplanar TEE has reduced the incidence of these aretefacts, but has not resolved the problem: the artefactual images are often found in different planes. Linear artefacts stem from multiple reflections of the ultrasound off the walls of the left atrium in particular. They arise in the presence of a wide aorta, with a diameter greater than that of the left atrium, with the ultrasound probe at a distance equal to or double the atrial diameter (Fig. 11.4). In fact, an aortic diameter of > 50 mm and a left atrium/ aorta ratio of < 0.6 are excellent predictive factors for the creation of artefacts.
Three principal types of artefact have been described that are due to the reflection of the ultrasound from either the posterior wall of the left atrium (type A), the posterior wall of the right pulmonary artery (type C) or the interaction between the two (type B). Type A linear artefacts, due to the reflection by the aorta/left atrium interface, are the most common. They may be easily identified by their particular echocardiographic appearance, especially when using M-mode (Box 11.2), which makes it possible to avoid an erroneous diagnosis of aortic dissection.
Box 11.2 Echocardiographic signs that suggest an ultrasound artefact simulating aortic dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree