Thoracic Abnormalities Associated With Acute/Chronic Liver Disease
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Varices
Alpha-1 Antiprotease Deficiency
Hepatic Hydrothorax
Noncardiac Pulmonary Edema
Less Common
Hepatopulmonary Syndrome
Portopulmonary Hypertension
Cystic Fibrosis
Hepatocellular Carcinoma Metastases
Sarcoidosis
Rare but Important
Lymphocytic Interstitial Pneumonia
Amiodarone Pulmonary Toxicity
Heterotaxy Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Elevated right hemidiaphragm may be secondary to underlying liver disease
Helpful Clues for Common Diagnoses
Varices
Most common complication of portal hypertension
Radiographic clues: Small liver, splenomegaly, lower paraspinal widening
CT: Serpiginous vessels surrounding thickened distal esophageal wall
Vessels may be unopacified on arterial phase imaging
Rarely, portal veins may decompress into pulmonary veins across pleural adhesions or inferior pulmonary ligament leading to right-to-left shunt
Splenopneumopexy: Obsolete surgical procedure of left hemidiaphragm with abrasion of spleen and left lower lobe allowing collaterals to develop
Alpha-1 Antiprotease Deficiency
Inherited (autosomal dominant) deficiency of alpha-1 antitrypsin (A1AT)
Hepatic A1AT expressed in liver, released into circulation
In deficiency, A1AT accumulates in liver leading to cirrhosis
5-10% of patients > 50 years old with A1AT have cirrhosis
CT: Panlobular emphysema, primarily in lower lung zones
Mild cylindrical bronchiectasis also common (40%)
Pulmonary function preserved until 5-6th decade in nonsmokers (3rd decade in smokers)
Emphysema major cause of death in smokers
Liver disease major cause of death in nonsmokers
Hepatic Hydrothorax
Definition: Pleural effusion in cirrhosis in absence of cardiopulmonary disease
Prevalence in cirrhotic patients (5-10%)
Right pleural effusion (85%), left (13%), bilateral (2%)
May occur in absence of ascites
Noncardiac Pulmonary Edema
Seen in up to 40% with fulminant hepatic failure
High mortality rate
Helpful Clues for Less Common Diagnoses
Hepatopulmonary Syndrome
Triad of chronic liver disease (usually cirrhosis), increased alveolar-arterial oxygen gradient on room air, intrapulmonary vascular dilatation
May be related to liver’s inability to break down circulating vasodilators (thought to be nitric oxide)
Prevalence 20% in those awaiting orthotopic liver transplantation
CT: Dilated peripheral arteries (2x larger than adjacent bronchi), primarily in lower lobes
V/Q scan: Macroaggregated albumin bypasses lungs and results in systemic activity in brain and kidneys
Reversible after orthotopic liver transplantation
Portopulmonary Hypertension
May be related to liver’s inability to break down circulating vasoconstrictive agents
Not related to severity of liver disease
Prevalence: 2-5% in patients with cirrhosis
CT findings identical to other causes of pulmonary hypertension: Enlarged central pulmonary arteries, attenuation of peripheral pulmonary arteries, mosaic attenuation
Mean survival 15 months
Relative contraindication to orthotopic liver transplantation
Cystic Fibrosis
Hereditary disorder (autosomal recessive) that affects chloride transport
Airways primarily affected
Bronchiectasis usually predominant in upper lobes
Up to 40% have focal biliary cirrhosis, 10% go on to develop biliary cirrhosis
Hepatocellular Carcinoma Metastases
Typical manifestation is multiple variable-sized pulmonary nodules
Proclivity of hepatocellular carcinoma to invade veins may give rise to intravascular metastases
Sarcoidosis
Drug complication of interferon therapy in patients with hepatitis C infection
Sarcoid primarily affects chest (75%) or skin
Radiographic findings identical to typical sarcoidosis, ranging from symmetric hilar adenopathy to perilymphatic nodularity
Helpful Clues for Rare Diagnoses
Lymphocytic Interstitial Pneumonia
Part of a spectrum of lymphoproliferative disorders
Association between primary biliary cirrhosis and Sjögren syndrome
CT: Ground-glass opacities (100%), poorly defined centrilobular nodules
Thin-walled cysts most distinctive finding (80%), involve < 10% of total lung, may be only finding
Amiodarone Pulmonary Toxicity
Antiarrhythmic agent with 3 iodine molecules
Toxicity is dose related and accumulates in liver and lung
Acute presentation: High-opacity areas of lung consolidation
Chronic presentation: Diffuse interstitial thickening
Heterotaxy Syndrome
Situs describes position of cardiac atria and viscera
Atrial situs best determined by location of liver
Situs ambiguous or heterotaxy syndrome
Asplenia: Right-sided symmetry
Polysplenia: Left-sided symmetry
If discordant location of stomach bubble and cardiac apex, then consider asplenia or polysplenia
Image Gallery
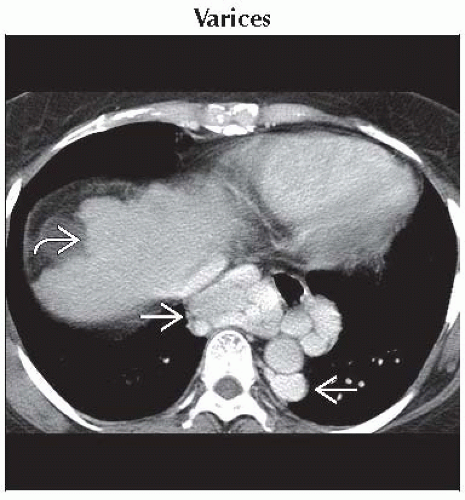 Axial CECT shows enlarged, contrast-enhancing paraesophageal varices
 . The liver is small and cirrhotic . The liver is small and cirrhotic  . Note that the varices are as large as the descending aorta. . Note that the varices are as large as the descending aorta.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|