Fig. 2.1
Positioning of the C-arm fluoroscopic unit during examination of a patient in the lateral fluoroscopic view. There is a disk of known diameter taped under the chin, a towel protecting the clothing from spilled barium, and a lead apron shielding the reproductive organs
The ability to record the studies at 30 fps and review in a frame-by-frame manner is essential for precise interpretation and analysis. Studies obtained at capture rates less than 30 fps may miss significant pathology. All examinations are reviewed weekly during an interdisciplinary panel that includes SLPs, nurses, physicians, students, and dietitians.
Patients are weighed, measured, and given the validated ten-item Eating Assessment Tool (EAT-10) prior to the administration of barium and the results are documented in the EMR (Fig. 2.2). The height and weight afford calculation of the BMI, which assists with the assessment of nutritional status. The association of patient symptoms captured by the EAT-10 with VFSS findings provides essential information to assist the clinician with the development of a comprehensive treatment plan. The EAT-10 documents the level of baseline disability and is instrumental in monitoring treatment efficacy.
Fig. 2.2
The ten-item Eating Assessment Tool (EAT-10)
We use a 60 % weight/volume (w/v) ratio of barium sulfate (Fig. 2.3; EZpaque, Westbury, NJ). This contrast agent has the rheological properties of a nectar thick liquid. The use of a nectar thick liquid for the VFSS has advantages and limitations. Higher density barium formulations (nectar and honey thick) are more viscous. The increased viscosity and subsequent mucosal adherence provides better visualization of subtle pathology such as webs, rings, and cricopharyngeus muscle bars that may otherwise be missed. The higher density barium is also more radiopaque and is easier to visualize under fluoroscopy . Less dense agents that behave like a thin liquid do not provide the anatomic detail nor possess the mucosal adherence of the thicker formulations. Although our protocol does not routinely utilize less dense, thinner barium for these reasons, we will, on occasion, dilute the suspension by 50 % using water. Patients at risk of aspirating thin liquids will have an increased likelihood of aspirating the thinner barium formulation. The information acquired from the thinner, less dense formulation may assist with treatment recommendations but it will also have direct implications on study analysis. All of the normative data for the objective fluoroscopic measures that we use (Chap. 7) are based on use of the 60 % w/v barium concentration. Altering the density of the barium will have a direct effect on deglutitive measures such as pharyngeal transit time and opening. This alteration will make the interpretation of objective fluoroscopic measures inaccurate. For this reason, we perform the majority of our VFSSs with the 60 % w/v formulation. It is essential that the clinician take the density of the barium into consideration when performing and analyzing these investigations. A comprehensive investigation of the benefits and limitations of precise barium formulations has not been conducted and warrants future study. Our experience suggests that the 60 % w/v formulation provides a balance between the desired rheology and the ability to provide optimal anatomic detail.
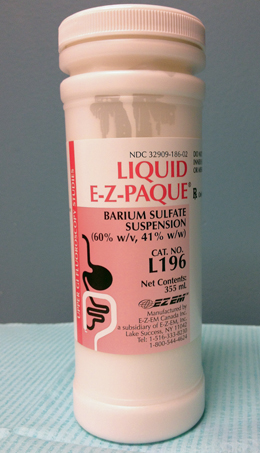
Fig. 2.3
Sixty percent weight/volume ratio of barium sulfate (EZpaque, Westbury, NJ)
The patient is positioned in an examination chair with the fluoroscopy unit in the lateral position. The patient head position is neutral and facing forward (Fig. 2.1). Clothing, jewelry, and other artifacts that may interfere with the fluoroscopic image are removed and stored. A lead apron is placed over the patient’s pelvic region to protect the reproductive organs and a towel is draped over the shoulders and lap to prevent drips of barium from getting on patient clothing. A radiopaque disk of known diameter (19 mm) is secured to the patient’s chin with tape to allow for later calibration during the on screen calculation of objective fluoroscopic swallow measures (Chap. 7). The boundaries of the fluoroscopy field in the lateral view are the lips anteriorly, nasopharynx superiorly, cervical spine posteriorly, and cervical esophagus inferiorly (Fig. 2.4). The boundaries of the fluoroscopy field in the anterior-posterior (AP) view are the walls of the pharynx laterally, the nasopharynx superiorly, and the cervical esophagus inferiorly (Fig. 2.5). The patient is positioned upright with the spine perpendicular and the chin parallel to the floor. A standardized position is essential. Subtle variations in head tilt or position may alter swallowing biomechanics and are to be avoided unless specific maneuvers are being tested.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


