Fig. 15.1
Images from perfusion-fixed hearts from the Visible Heart® Laboratory’s library: (1) calcified aortic valve (upper left panel), (2) pulmonary valve (upper right panel), (3) subvalvular apparatus of the mitral valve (lower left panel), and (4) tricuspid valve from the right ventricle (lower right panel). Modified from The Atlas of Human Cardiac Anatomy [14]
To date, our library of more than 250 hearts continues to provide researchers with information on how potential valve therapies/technologies may interact with the surrounding cardiac anatomies. In addition to anatomical investigations, such resources allow for the placement of prototype devices and the rapid comparison of how given devices interact with human specimens exhibiting different cardiac pathologies [12, 13]. Fresh cadaver hearts received by the Visible Heart® laboratory are documented at each stage of the acquisition process to record any global anatomical changes during the fixation process, such as tissue weight and overall dimensions. Images of the fresh preparation, the resulting fixed specimen, and the nondestructive imaging of one specimen from the library (adapted from the Atlas of Human Cardiac Anatomy [14]) can be seen in Fig. 15.2.
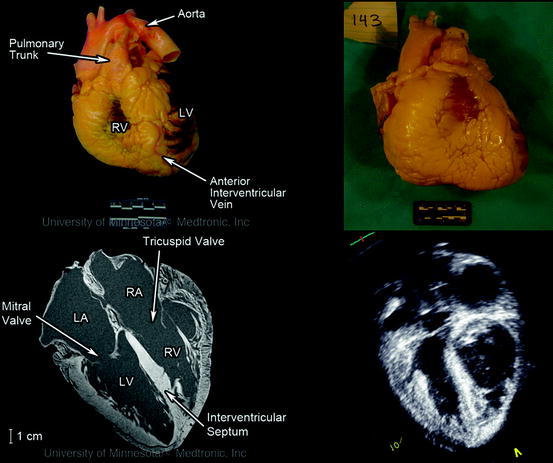
Fig. 15.2
Images of a heart received by the Visible Heart® library and imaged fresh (upper left panel), after perfusion fixation (upper right panel) and scanned in a 3 T Siemens MRI scanner (bottom left panel) and GE Vivid I ultrasound (lower right panel) in the 4-chamber long-axis view. Modified from The Atlas of Human Cardiac Anatomy [14]
Recent advances in high-resolution noninvasive cardiac imaging have fostered extensive work in the in vivo analyses of anatomical variations from patient to patient using a variety of imaging modalities:
Nondestructive imaging of specimens from the Visible Heart® library via ultrasound, CT, and MRI has been used to collate a digital database of these hearts for educational and research purposes. The perfusion-fixed specimens are prepared by suspending them in a gel medium, allowing for a full complement of multimodal imaging to be performed on the hearts without changing the orientation [19]. Obtaining high-resolution images has allowed for detailed analyses of cardiac anatomies for a variety of both normal and pathologic specimens; this imaging is considered not possible with available clinical imaging protocols. Such studies have included (1) the characterization of the positions and sizes of the papillary muscle complexes within the left ventricle for dilated and hypertrophic cardiomyopathy specimens [14] and (2) the analyses of fiber orientations of specimens obtained from patients in end-stage heart failure, using diffusion tensor MRI [20]. In addition, it has been possible to compare the ability of different imaging modalities to assess the anatomical characteristics of specific cardiac pathologies, such as aortic stenosis [21], thus building on the work of other researchers [22].
15.4 In Vitro Isolated Heart Models
A comprehensive understanding of the cardiac valve anatomy provides device designers with fundamental information regarding the anatomical dimensions and variations of the environment into which the device or therapy will be delivered. However, these static human heart specimens do not address the complications surrounding the delivery and function of a device or therapy in a beating heart. Before embarking upon complex and expensive chronic animal testing protocols which are required to prove the efficacy of novel prosthetic valves, there is exceptional value in testing cardiac devices in reanimated beating heart models. The Visible Heart® laboratory at the University of Minnesota has reanimated over 1,000 large mammalian hearts (canine, ovine, swine, mini-pigs, and human) for such studies in the last decade. There have been several other academic institutions and private companies that have developed in vitro large mammalian heart models, with many groups effectively developing systems based upon the mechanical reanimation of cadaveric large mammalian hearts. For example, Richards et al. were able to consistently and reliably quantify mitral regurgitation across a range of severities in explanted porcine hearts and investigate the efficacy of various repair techniques [23]. Further, two other groups have succeeded in studying the electrophysiology of explanted human hearts by sustaining the heart with a pressurized coronary flow of oxygen saturated salt solution via Langendorff perfusion [24, 25]. However, it should be noted that the true “reanimation” of large mammalian hearts (whereby the heart functions independently of any mechanical or electrical assistance) has only been achieved by a small number of research groups. Araki et al., Nagoya University, Japan, reported that they were able to complete optical and hemodynamic analyses of cardiac valves in reanimated swine hearts [26]. Most recently, Weger et al. at the Leiden University Medical Center, Netherlands, have monitored transcatheter valve implantations in reanimated swine hearts using their described PhysioHeart system [27]. However it should be noted that in both of these aforementioned preparations, the researchers were limited by the amount of time the heart remained viable, a factor considered key to the accessibility of the heart for device testing.
The Visible Heart® laboratory partnered with Medtronic, Inc. in 1997 to develop the Visible Heart® methodologies which consist of a large mammalian isolated heart model that can be controlled to function in either Langendorff [25], right-side working, or four-chamber working modes [28]. Over this time and continuing today, the laboratory has been developing/optimizing this apparatus for reanimating hearts whereby isolated large mammalian hearts are perfused and then actively pump a clear crystalloid perfusate in the place of blood. Images of a human heart connected to the Visible Heart® apparatus can be seen in Fig. 15.3. This approach has allowed our group to visualize what occurs inside the heart during device deployment procedures, and subsequently to determine how such devices interact with the specific anatomies of the heart throughout all the phases of the cardiac cycle.
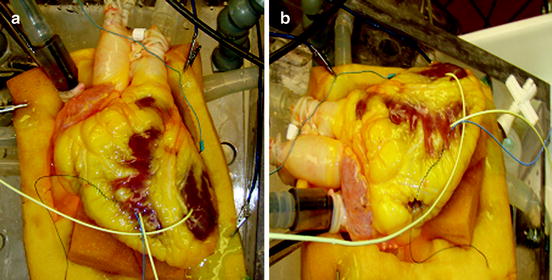
Fig. 15.3
Images of a human heart connected to the Visible Heart® apparatus from an approximation of the anterior-posterior aspect (a) and from the left anterior oblique aspect (b)
Briefly, the approach includes the initial step of removing the heart using standard cardioplegia procedures [28, 29]. Once isolated, cannulae are inserted into the great vessels allowing the placement of endoscopes or devices into all four working chambers. Following reanimation, cardiac and systemic pressures and outputs can be monitored and preloads and afterloads adjusted accordingly, as described by Starling’s law of the heart; one can also simulate pathologies such as hypertension. Additionally, the isolated heart apparatus allows researchers to quickly switch the perfusion system to operate in Langendorff, right-side working, or four-chamber working modes. During the Langendorff mode, the left-side afterload is held constant with a coronary perfusion pressure of approximately 60 mmHg [28]; thus, the flow through the coronaries is determined by dilation or constriction of the coronary arteries. Right-side working mode combines Langendorff retrograde aortic perfusion with antegrade, or physiologic, flow through the right atrium and right ventricle (adjustable between ∼3 and 5 L/min). During four-chamber working mode, the flow through a heart is normally determined by its intrinsic heart rate, preloads, afterloads, and the relative contractilities of the various heart chambers. By controlling the orientation of the heart in the apparatus and determining the preload and afterload pressures exerted on the specimen, we have observed that we can recreate specific cardiac states. Interestingly, the intrinsic heart rate and hemodynamic performance can be modified by altering the temperature of the buffer or by adding pharmacological agents (e.g., catecholamines, calcium, or anesthetics), which are discussed later in this chapter. Although no model can perfectly mimic in vivo conditions, to date the apparatus has allowed researchers to simulate a broad range of particular physiological environments that are observed in various clinical settings.
15.5 How Can an Isolated Heart Preparation Augment and Complement Benchtop Testing?
The combination of a “live” functional anatomy within a controlled “benchtop” experimental setting provides a unique stepping stone between in vitro device testing and in vivo implantations required for implantable medical devices. Figure 15.4 shows how the typical stages of device testing and development compare in terms of the relevance of the testing environment to the intended functional environment, the quantity of data one can reasonably expect to collect, and the estimated cost of performing such investigations. It can easily be observed that as the relevance of a particular testing methodology increases, the relative costs will also dramatically increase; thus, the likely number of possible iterations decreases. Consequently, any possible augmentations to device testing prior to chronic animal implants (e.g., via isolated beating heart preps) can, in turn, greatly reduce the overall product development costs and speed clinical uses of novel valve repair, implants, and their associated delivery systems.
Fig. 15.4
Proposed hierarchy between the relevance of various experimental approaches, the amount of data one can obtain, and the relative costs. Thus, e.g., if you wish to perform medical device design research in the field of prosthetic valves, ideally you would like to perform human trials in vivo, but this not only raises medical ethical issues, but is highly costly and may provide useful data for one specific valve design and procedure. Whereas if you move the research approach downward, i.e., employ an isolated large mammalian heart model in vitro, you can obtain more data at a lower cost, but then you must justify the appropriateness of the chosen model. Yet, in one given study it may be possible to perform multiple procedures for comparisons or at least multiple implants in multiple hearts with fairly consistent anatomies
Accelerated wear testing and fatigue testing are required gold standards for the assessment of cardiac valve durability (see Chaps. 12–14, 16, 17). As such, in accelerated wear testing the hydrodynamic conditions are tightly controlled and easily varied, allowing the durability of the valve leaflets to be assessed under a variety of predetermined conditions. Similarly, the boundary conditions imposed on the valve frame or commissure posts during fatigue testing can assess frame durability. Isolated heart preparations, including the Visible Heart® methodologies, will never replace these forms of testing, but unique information regarding the device-tissue interactions in the later can be observed. It should be noted that since the hydrodynamics of isolated heart preparations are typically less aggressive environments than what is experienced during accelerated wear testing, the boundary conditions observed for a device in such studies are not directly transferable to accelerated wear testing test fixtures. Yet on the other hand, they can serve as means to obtain additional information to ascertain the validity of any boundary conditions within the accelerated testing protocol. More specifically, in fatigue testing the frames should be tested to the anticipated worst-case conditions, which would not likely be observed in the Visible Heart® apparatus. Nevertheless, observations from the Visible Heart® approach, in which the implanted device can be directly visualized, have helped to ensure that all forms of boundary conditions have been taken into account. Most importantly, such experimentation has provided us with a so-called physiological link between benchtop testing of devices and animal testing. In other words, acute phenomena observed during accelerated wear testing and the insights gained with both invasive and noninvasive imaging techniques in animal studies may be directly observed during a valve implant study in vitro. For example, a procedural issue observed under fluoroscopy during an in vivo animal implant could be recreated by employing the Visible Heart® approach (under direct visualization) with simultaneous fluoroscopy, thus gaining a better understanding of potential adverse issues. We consider that having the Visible Heart® apparatus as a tool for device design has allowed us to obtain a more rapid understanding of phenomena observed in both benchtop and preclinical settings; as such, it is an invaluable tool for a device designer, especially at the early stages of development.
15.6 The Importance of Species Selection in In Vitro Cardiac Valve Research
The ultimate utility of studies performed with Visible Heart® methodologies, such as transcatheter valve development, is in part determined by the heart chosen for reanimation. We suggest that the criteria for species selection for acute in vitro studies are slightly different from those for chronic valve assessments (Chap. 16) due to the elimination of all systemic factors that may contribute to device performance. In other words, the species of the donor can be chosen specifically for its relative cardiac anatomy rather than for factors such as thrombogenesis, immune response, and/or growth rates.
For years, the canine heart has been used for such experimentation and has provided useful information. Yet it should be recognized that canine hearts have an unusually large amount of collateral coronary circulation (similar to humans in end-stage chronic heart failure), and this in turn results in the inconsistent creation of ischemic (infarct) regions [30]. Sheep have been historically employed for chronic valve implantation studies, as valve function and valve orifice sizes observed in sheep are very similar to those of a human heart. Additionally, the relatively large atria of the sheep’s heart allow for straightforward surgical approaches to the atrioventricular valves. However, it has recently been proposed that swine are an excellent model for acute cardiac device testing, as porcine hearts have very similar anatomies to those of humans with respect to the cardiac valves, conduction system, coronary arteries, and great vessels. Nevertheless, it is important to note that there are some specific variations in animal valve anatomy that should be known; such interindividual and interspecies variations have been extensively researched by Michaëlsson and Ho [31], and other investigators have highlighted the impact of such work in medical device testing [28–30, 32]. For example, when testing aortic valve therapies in the swine model, it should be considered that there are several interspecies differences in leaflet morphologies and coronary ostia positioning, resulting in an increased likelihood of interaction between these two structures [30]. Additionally, in swine (1) the ascending aorta is typically shorter, i.e., the branch of the brachiocephalic artery and the start of the aortic arch are closer to the aortic annulus than in humans; (2) there are only two primary arteries exiting the arch; and (3) there typically are no plaques present or calcific stiffening of the aorta [30]. Anatomical variations in the mitral and tricuspid valve anatomies are also noteworthy, e.g., there can be primary differences in the number of leaflets and the structures of the subvalvular apparatus. Interestingly, these variations are more often attributed to interindividual differences rather than interspecies variation [30, 31].
Importantly for those interested in transcatheter-delivered valves, the relationship between the various valves themselves and the cardiac conduction system is comparable between swine and human anatomies. Hill et al. have theorized that the interaction between an aortic prosthesis, the mitral valve, and the conduction systems within the interventricular system can be quantified to a reasonable extent in the swine model [30].
Due to their specific anatomical similarities with human hearts and the relative ease of procurement (excision and reanimation), the mainstay of cardiac valve research done in the Visible Heart® laboratory is completed using swine hearts. Nevertheless, as previously mentioned, the laboratory has also had the privilege to obtain fresh human heart specimens for reanimation, for both educational and research purposes. Such hearts, if received in a timely manner and with complete anatomies including the great vessels, have been reanimated using the same methodologies as previously described for swine hearts. By reanimating these hearts using a clear perfusate, visualization of the internal cardiac anatomy has provided novel insights into the relative variations of human cardiac anatomies (in healthy individuals), and has highlighted the alterations that occur with various pathologies. Finally, this approach provides the unique opportunity to deliver existing or novel devices within functional human anatomies without the concerns and considerations required in clinical trials; thus it has allowed researchers to garner invaluable knowledge about their device designs that otherwise could not be generated using animal models.
15.7 Understanding and Controlling Heart Function In Vitro
When studying cardiac valves, it is important to understand how the heart functions in both systole and diastole (Chaps. 1 and 2). When working with a specimen in vitro, the performance of the reanimated heart can be influenced by several additional mechanisms. For example, subsequent cardiac function will be compromised by the amount of cell injury that occurs, governed in part by the amount of time between heart explant and reanimation. It is considered that if this period exceeds 6 hours, performance will be compromised, even if the heart is stored under ideal conditions. To reduce such time-associated myocardial injury due to global ischemia, the Visible Heart® laboratory has investigated the use of cardioprotective agents delivered before explanting the heart [33]. Most recently, the laboratory have been investigating the effect of omega-3 polyunsaturated fatty acids administered before explant on the acute function upon reanimation.
Because of the isolation process, the reanimated heart has no direct parasympathetic or sympathetic innervation and thus is not affected by any signals from the autonomic nervous system. However, pharmaceuticals/hormones such as dobutamine and epinephrine can be administered to the circulating perfusate. These catecholamines work by stimulating the β1-receptor on the myocytes, acting as chronotropes and inotropes, and increasing heart rates and contractility and thus overall cardiac output. Furthermore, the ionic balance of the circulating buffer can have very dramatic effects, e.g., increasing the calcium (Ca2+) concentration in the buffer will act as a potent inotrope by increasing the Ca2+ inside the cell during the action potential. The laboratory will often utilize such inotropic agents shortly after deploying a valve within an isolated heart to increase cardiac output and ejection fraction and therefore optimize function of the implanted prosthesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


