Chapter 25 The Surgeon’s Role in Mass Casualty Incidents
Key Concepts
Classification of Disasters and Implications for Trauma Care
In a mass casualty incident (MCI), a medical system is suddenly confronted by a large number of casualties needing care within a short period of time. This unexpected surge creates a discrepancy between the number of patients and the resources available to treat them. An MCI can be classified by cause (natural versus man-made), duration, location, and many other characteristics, but there is no single universally accepted classification of disasters. From the clinical perspective of medical care, it is important to distinguish among three classes of disaster scenarios and understand the implications for trauma care (Table 25-1).1,2
Table 25-1 Classification of Disasters and Implications for Trauma Care
| DISASTER CLASS | TOTAL NUMBER OF CASUALTIES | IMPLICATIONS FOR TRAUMA CARE |
|---|---|---|
| Multiple casualty | Less than ED capacity | Standards of care are maintained for all severe casualties. |
| Mass casualty | More than ED capacity | Care of some severe casualties is delayed or suboptimal. |
| Major disaster | ED and hospital overwhelmed | Most severely injured patients die or survive without any medical care. |
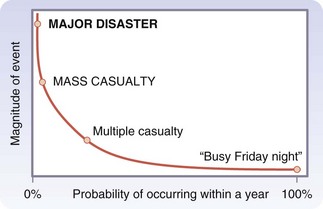
Major Medical Disasters
The magnitude of a MCI is inversely related to its frequency (Fig. 25-1). The overwhelming majority of practicing surgeons will not encounter a major medical disaster in their communities, whereas most hospitals occasionally face limited multiple casualty incidents. In fact, busy Friday nights, a single trauma team on call coping with a cluster of severely injured patients arriving together is situation that occurs frequently in every urban trauma center. It represents the lowermost end of a spectrum of magnitudes, with a major earthquake or a devastating Tsunami at the other extreme. The sad paradox of disaster preparedness is that the most time and effort is spent on preparing and training for the largest and least likely doomsday scenarios instead of improving the response to limited but more realistic threats.
Injury Severity Distribution
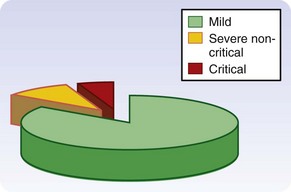
A key feature of every MCI is the injury severity distribution of the casualties. Regardless of the cause or magnitude of the MCI, only about 10% to 15% of survivors presenting to a hospital will be severely wounded, of whom roughly one third will have immediate life-threatening injuries (Fig. 25-2). Most others sustain minor trauma or nonurgent injuries.3 For example, during the London subway bombings in July 2005, the Royal London Hospital received 194 casualties within 3 hours, but only 27 (14%) were severely injured. Of these, only 8 casualties (4% of the total) were critically wounded.4 Although the death toll at the scene depends on the cause of the MCI, and is very high when structural collapse is involved, the injury severity distribution is a constant feature of MCIs. This means that even though the total number of casualties may be high, the overwhelming majority will not require a high level of trauma care and are not urgent. These considerations form the rationale for planning an effective medical response.
Mass Casualty and Modern Trauma Systems
Goal of the Hospital Disaster Responses
Bearing in mind the injury severity distribution, a MCI is “a needle in a haystack” situation in which a small group of severely injured patients who require immediate high-level trauma care is immersed within a much larger group of casualties with minor injuries, who can tolerate delays and even suboptimal care without adversely affecting their outcome.1 The ultimate goal of the entire hospital disaster response is, therefore, to provide this small group of critically injured patients with a level of care that approximates the care provided to similarly injured patients on a normal working day. This goal has never been formally declared by the American College of Surgeons2 or any other professional organization, but it has always been implicitly understood by surgeons and trauma care providers and is certainly an expectation of the public. In a multiple casualty incident, this goal can be achieved by effective triage and priority-driven trauma care. In a mass casualty incident, it can still be achieved by diverting trauma assets and resources from the less severely injured to the critically wounded—but at a cost. Contrary to popular belief, the casualties whose management is delayed and compromised in a mass casualty scenario are not the mild ones but the severely injured patients with non–life-threatening injuries.
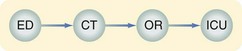
The Trauma Service Line in Disasters
Every modern trauma center establishes and maintains a dedicated trauma service line for severely injured patients during normal daily operations (Fig. 25-3). This service line includes trauma teams, assets, and facilities (e.g., resuscitation bays and operating rooms), all readily available to treat seriously injured patients. The trauma service line of a hospital provides the resources for optimal care of individual patients, but has limited capabilities to treat multiple badly injured patients simultaneously. The goal of an effective disaster response is therefore to preserve the hospital trauma service line in the face of an unusually large number of casualties. From the trauma care perspective, success in dealing with an MCI is not streamlining the flow of 40 or 60 casualties through the ED, but rather preserving the capability to provide optimal trauma care to the three or four critically injured (but salvageable) casualties among them.5
Casualty Load and Surge Capacity
Many hospital administrators have an exaggerated view of the capacity of their institutions because hospital disaster planning is typically based on counting ED gurneys and hospital beds, rather than on the rate at which casualties are treated (or processed) by the hospital trauma system. In reality, as the MCI unfolds and progressively more casualties arrive, finding an available resuscitation bay and staffing it with experienced trauma teams becomes increasingly difficult.1
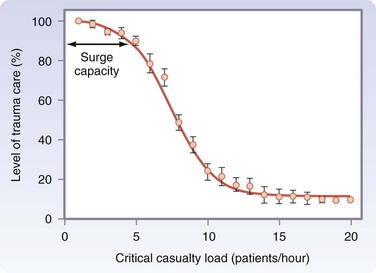
From the trauma care perspective, the arrival rate of severe casualties is a more meaningful metric of the burden on a trauma system than the absolute number of casualties. The casualty load is the arrival rate of severe casualties per hour, and an increasing casualty load eventually leads to degradation of trauma care as severely injured patients compete for the limited assets and resources. An intact trauma service line provides each severe casualty with a trauma team, resuscitation bay, and other resources, such as an available computed tomography (CT) scanner, operating room, and intensive care bed. The point beyond which this level of care cannot be maintained for new arrivals represents the surge capacity of the trauma service line of the hospital.6 Surge capacity is, therefore, a dynamic measure of the processing capacity of the trauma service line, and cannot be derived from static calculations of ED gurneys and staff. Using a similar definition, a surge capacity can also be defined separately for each trauma-related facility in the hospital.
An increasing casualty load adversely affects the quality of trauma care for the severely injured because many casualties compete for the same limited trauma assets and resources. Analysis using a computer model6 describes this relationship as a sigmoid-shaped curve (Fig. 25-4). The upper flat portion of the curve represents an intact trauma service line, where the level of care for severe casualties approximates the care given to a single patient on a normal working day. This is a multiple casualty incident. The steep portion represents a gradually failing trauma service line, corresponding to a mass casualty scenario. The lower flat portion represents a failed (or nonexistent) service line overwhelmed by a major medical disaster.
The surge capacity of the trauma service line is the point beyond which the level of care begins to drop. An effective disaster response shifts the curve to the right, increasing the surge capacity and resulting in a more gradual degradation of the level of care. An empirical estimate7 puts the surge capacity at one severely injured patient per hour for every 100 hospital beds, providing a practical yardstick that can be used in disaster planning.
Mass Casualty and Modern Trauma Systems
The overwhelming majority of urban terrorist bombings are multiple casualty incidents that do not exceed the surge capacity of individual hospitals. However, in the past decade, terrorist groups have made repeated attempts to increase the magnitude of these MCIs by coordinated multiple simultaneous bombings. The two best documented examples were the Madrid trains bombing (March 2004)8 and the London subway bombing (July 2005).4 However, these incidents clearly demonstrated that modern emergency medical services (EMS) and trauma systems in large metropolitan areas serve as effective buffers that mitigate the medical impact of a large-scale event by distributing casualties among hospitals. With 2253 casualties in Madrid and more than 700 in London, rapid dispersion of the casualties among several hospitals resulted in each participating hospital facing only a multiple casualty incident with a handful of critical patients. This strong buffering mechanism was, however, conspicuously absent in the U.S. Embassy bombing in Nairobi, Kenya, in 1998, where more than 4000 casualties flooded the Kenyatta National Hospital.9 This inadequately documented MCI is the only truly overwhelming urban mass casualty incident in recent history. This is a key point that is worth reemphasizing: no hospital in a metropolitan area that has a functioning EMS system has ever been overwhelmed by a MCI.
Medical Care at the Scene
Most MCIs in an urban environment follow a typical timeline that can be divided into four distinct phases (Table 25-2).10 The initial chaotic phase begins immediately after the inciting event. Without any organized medical effort, many minor casualties and those with acute stress reaction run from the scene and find their way to the nearest hospitals. The organized effort phase begins when a prehospital responder takes charge at the scene and initiates a systematic medical effort while also ensuring the safety and security of the medical teams. The most important aspect of this phase is effective field triage, which allows priority-driven transport of casualties to hospitals. This is followed by the site-clearing phase, the duration of which depends on the specific circumstances of the incident (i.e., magnitude, structural collapse, or need for prolonged extrication). It ends when the last live casualty is transported from the scene. The late phase is a poorly defined period when minor casualties who initially ran from the scene decide to seek medical attention, often after being persuaded by family and friends.
Table 25-2 Typical Timeline of Urban Mass Casualty Incident
| SCENE PHASE | CHARACTERISTICS | IMPLICATIONS FOR THE ED |
|---|---|---|
| Chaotic | No organized medical care; mild casualties go to nearest hospital | First wave: A few walking wounded |
| Organized effort | Key is effective triage; priority-driven transport of casualties | Second wave: Main body of casualties |
| Site clearing | Remaining casualties transported | |
| Late | Sporadic mild casualties | Third wave: Slow trickle of mild casualties |
From the hospital perspective, this timeline translates into a characteristic casualty arrival pattern consisting of three waves (see Table 25-2). The first wave consists of a small cluster of casualties with minor injuries who arrive in hospital on their own. After a variable interval, the main body of casualties begins to pour in, presenting a wide variety of injury severities. Finally, a slow trickle of late arrivals with minor injuries or acute stress reaction continues over many hours.10
Field triage schemes are based on a rapid assessment of clinical and physiologic parameters. Until recently, the dominant algorithm in the United States was START (simple triage and rapid treatment), which sorts casualties into four categories—immediate, delayed, minor, and deceased.11 Criticism of START, which results in excessive overtriage, has led to the recent introduction of the SALT triage scheme (sort, assess, life-saving interventions, treatment and/or transport), which combines global assessment of the casualties (e.g., walking versus laying still) with a more detailed yet brief assessment of vital signs.12 SALT has been endorsed by the American College of Surgeons and other professional organizations dealing with mass casualty triage. Although it is promoted as a universal triage scheme for MCIs, its main usefulness is at the scene rather than for hospital triage at the ED door.
Clinical Aspects of Hospital Disaster Plans
Hospital Disaster Response
Full activation of the entire disaster plan of a large hospital takes time, disrupts normal daily activities, is expensive, and is also usually unnecessary, because the overwhelming majority of MCIs that any hospital is likely to face are limited events. It makes sense, therefore, to base the hospital disaster plan on a tiered response.13 The plan for a limited MCI centers primarily on the ED and relies on in-house staff and resources. A plan for large-scale MCIs recruits reinforcement staff and additional facilities outside the ED. Although this tiered approach is not yet a formal part of the hospital disaster planning in the United States, it makes clinical and administrative sense and is implicitly adopted by a growing number of institutions.
From the perspective of trauma care, the hospital response consists of two distinct phases.10 During the initial phase, the incident is still evolving, casualties are arriving, and their ultimate number is unknown. Therefore, the key consideration is to preserve the trauma service line for the next critical arrival. The definitive phase begins when casualties are no longer arriving, the overall casualty number is known, and the hospital response envelope has been fully deployed. The clinical focus shifts to providing definitive care to all casualties in a graded, priority-oriented fashion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree