The Second Heart Sound
NORMAL S2
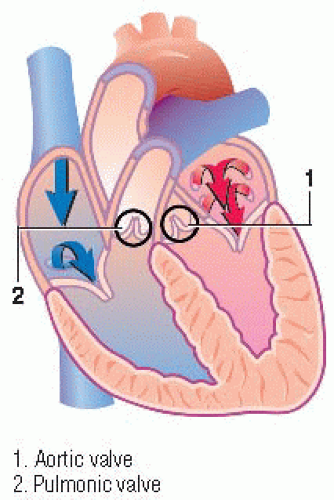
The cardiac vibrations associated with the closure of the aortic and pulmonic valves produce the second heart sound, S2. S2 is usually louder than S1 at the heart’s base and usually slightly higher in pitch than S1 at the heart’s apex.
S2, like S1, has two basic components: the aortic (A2) component and the pulmonic (P2) component. Both valves close at the end of ventricular systole. Normally, the aortic valve closes slightly ahead of the pulmonic valve.
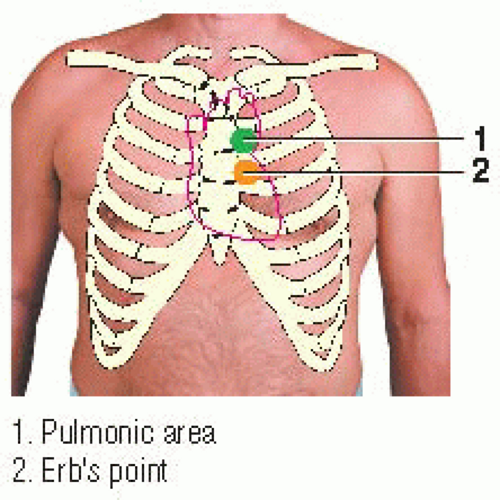
The closing pressure is higher in the aorta than in the pulmonary artery; therefore, A2 usually occurs earlier and is louder than P2. (♦Sound 5) Furthermore, A2 can be heard over the entire precordium, whereas P2 is usually auscultated over the pulmonic area.
Auscultatory area and relationship to ECG
To hear both components of S2, listen carefully with the diaphragm of the stethoscope over the pulmonic area. Listen for S2 just after the T wave in the patient’s electrocardiogram (ECG).
Sound characteristics
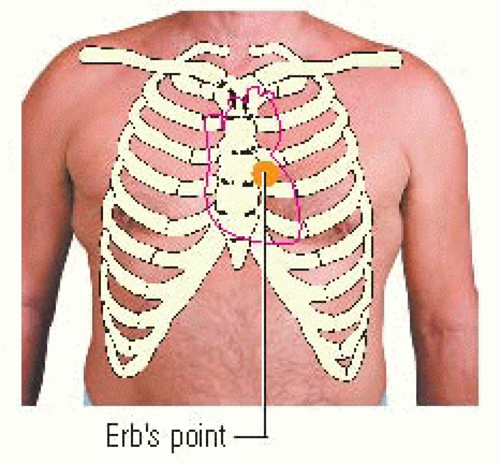
S2 is usually heard best near the heart’s base, over the pulmonic area or over Erb’s point. Its intensity directly relates to the amount of closing pressure in the aorta and pulmonary artery. S2 is slightly shorter in duration than S1. You can hear its high pitch best with the diaphragm of the stethoscope. The quality of S2 is somewhat booming; its timing coincides with the end of ventricular systole. (♦ Sound 5)
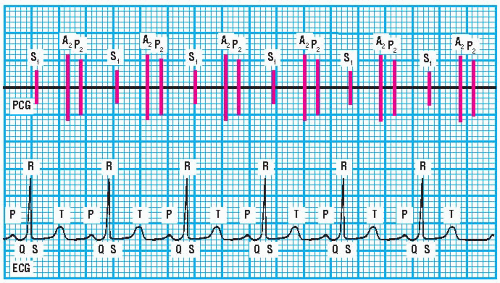 PCG and ECG showing S2 |
S2 SPLIT SOUNDS
Normal S2 split
The splitting of S2 into the A2 and P2 components is heard best during inspiration over Erb’s point.
Normal splitting of S2 in children may be heard in the second left intercostal space. The splitting of S2 in elderly persons may be more difficult to hear because of the widening of the anteroposterior chest diameter.
Remember, inspiration causes an increase in the venous return to the right side of the heart. This increased venous return prolongs the right ventricular ejection time. Inspiration also reduces pressure in the pulmonary artery, resulting in a delayed P2 or closure of the pulmonic valve. A decrease in blood flow to the left side of the heart occurs simultaneously, resulting in a shorter left ventricular ejection time.
Therefore, A2 is heard earlier than P2. (♦Sound 6) This means that a normal S2 split is heard during inspiration, and the A2 and P2 components fuse during expiration.
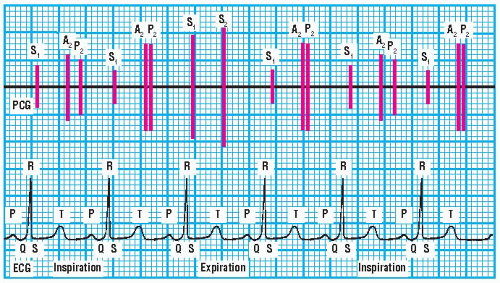 PCG and ECG showing respiratory changes in normal S2 split |
While listening to S2, you must determine the intensity of the A2 and P2 components and note the duration of the A2-P2 interval as well as its relationship to the respiratory cycle. (♦Sound 6) You should also document the S2 split, noting whether the A2-P2 interval increases or decreases during inspiration and expiration.
Changes in A2 and P2 intensity
The intensity of A2 and P2 changes proportionally with the difference in pressure gradients across the closed aortic and pulmonic valves. For example, P2 may be louder than normal in conditions associated with elevated pulmonary artery diastolic pressure, as occurs in some patients with heart failure, mitral stenosis, Eisenmenger’s syndrome, or other congenital heart diseases. When P2 increases in intensity, it’s sometimes heard over the mitral area and along the left sternal border. (♦Sound 7)
A2 intensity increases when diastolic pressure in the aorta increases. (♦Sound 8) This commonly happens during exercise; during states of excitement such as extreme fear; in hyperkinetic conditions, such as thyrotoxicosis, fever, and pregnancy; and in systemic hypertension. However, if the patient has left ventricular decompensation, ventricular relaxation is slower, and the pressure gradients may not be great enough to produce an accentuated A2.
Conversely, A2 intensity may be diminished in conditions that alter the development of diastolic pressure gradients, such as aortic regurgitation and hypotension. (♦Sound 9) A2 intensity also decreases when ventricular dysfunction is present, such as after an acute myocardial infarction. With this condition, P2 may become louder if the pulmonary artery pressure rises and systemic pressure falls. A2 is also softer or absent when aortic valve motion is restricted, as in severe aortic stenosis.
Abnormal S2 splits
Abnormal splitting is related to valvular dysfunction to alterations in blood flow to or from the ventricles, or to both. These changes may cause the normal S2 split to be absent during both phases of the respiratory cycle. Thus, only a single S2 is heard over Erb’s point. In another case, the split sounds may persist through inspiration and expiration with little or no respiratory variation. (♦Sound 10) The split sounds may also be heard paradoxically on expiration. The A2-P2 intervals vary, as does the intensity of A2 and P2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree