(1)
Department of General surgery, Fuwai Hospital, Beijing, China
4.1 General Considerations
4.1.1 Position
The two ventricles of the heart are separated by an interventricular groove. The right ventricle (RV) is located anterosuperior to the LV. The left anterior descending artery (ADA) runs in the anterior interventricular sulcus and supplies blood for the anterior portion of the interventricular septum. The posterior descending artery (PDA) runs in the posterior interventricular sulcus to the apex of the heart and supplies blood for the posterior portion of the interventricular septum. The right atria are separated from the RV by the right atrioventricular groove. The RCA travels down the right atrioventricular groove, toward the crux of the heart.
4.1.2 Structural Characteristics
In contrast to the LV, the RV is thin walled and compliant, and it can sustain only the low pressure of pulmonary circulation. The LV is circular shaped with thick walls and bears the high pressure of the systemic circulation. The ventricular septum is considered as part of the LV. In the systolic phase, the LV makes a concentric movement. Because the contractile force of the RV is weaker than that of the LV, the RV bears a lower pressure of pulmonary circulation. Hence, when the pulmonary artery pressure is elevated or the blood flow in the right heart increases, the RV is prone to failure. Therefore, surgery in this area should be avoided to reduce damage to the right ventricular structure. A right atrium and main pulmonary artery incision can be chosen in certain right ventricular cavity operations.
Other characteristics of the RV include the TV as the inflow entrance, the pulmonary valve as the outlet, a trabecular portion with many muscle bands, and the absence of a continuous fibrous connection between the tricuspid and pulmonary valves. The tricuspid and pulmonary valves are separated by infundibular muscle bundles that include a septum band on the right-side surface of the ventricular septum and a parietal band on the inner surface of the insolated wall of the RV. Compared to the LV, the RV has more muscle tissue between the inflow and outflow tracts (Fig. 4.1a, b).
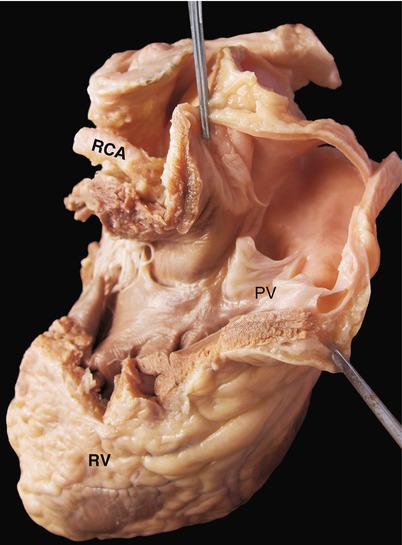
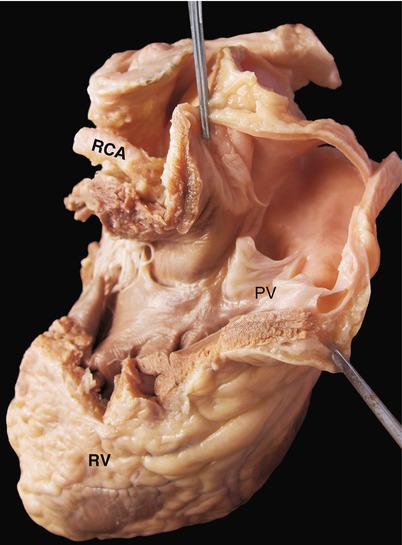
Fig. 4.1
(a) Pulmonary valve adjacent structures. The pulmonary and tricuspid valves are separated by the infundibular muscle. It is the important characteristics for determining if the arterial location relationship is normal. The left coronary artery lies in the back of the main pulmonary artery. (b) Muscle band under the main pulmonary artery (white arrow). The inner wall in this part of the heart usually is filled with small trabeculae muscles in the normal heart, but infundibular muscular hypertrophy can lead to pulmonary subvalvular stenosis
4.2 Right Ventricular Wall and Surgical Approaches
As the most anterior part of the heart, the anterior wall of the RV is easily exposed. Therefore, it is the first choice for making the right ventricular incision; however, to avoid injury to the anterior papillary muscle and the moderator band, the cardiac surgeon must be certain of the structure of RV before cutting it open. The anterior right ventricular wall can be divided into three regions: the conal part, the sinus, and the trabecular, as shown in Fig. 4.2. An incision made in the conus arteriosus (indicated by “C” in Fig. 4.2) is appropriate (Fig. 4.2). An incision can be made at the upper half of the right ventricular anterior wall; however, because the tricuspid anterior papillary muscle attachment point and the complex trabecular structure are found in the lower right corner, an incision should not be made in the region(Fig. 4.3).
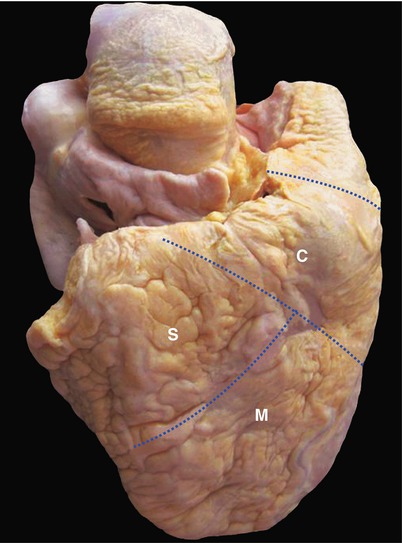
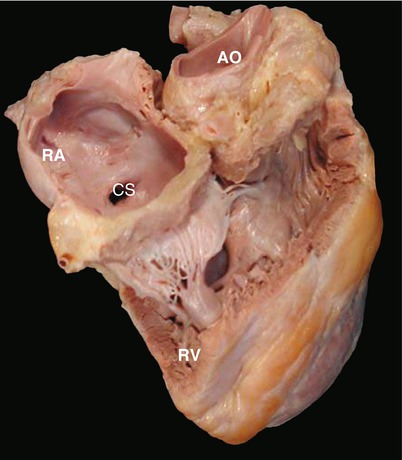
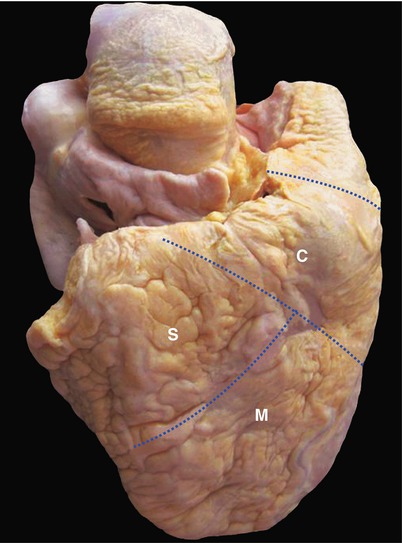
Fig. 4.2
Right ventricle. This specimen displayed by the frontal anatomical position shows the right ventricular anterior wall. Between the interventricular sulcus and the LV, the left anterior descending coronary artery runs within the interventricular groove. Between the atrioventricular groove and the right atrium, the right coronary artery runs within the atrioventricular groove. The aortic root is covered by the upper edge of the right ventricle. The anterior right ventricular wall can be divided into three parts: the conus arteriosus (C), the sinus (S), and the trabecular muscle (M)
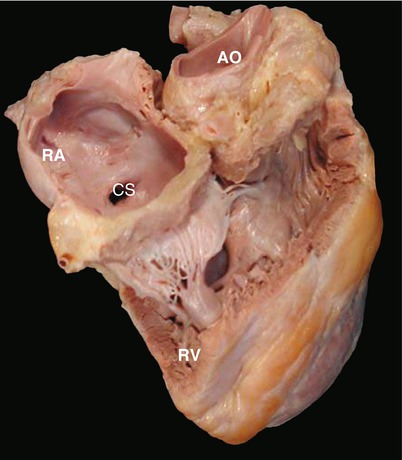
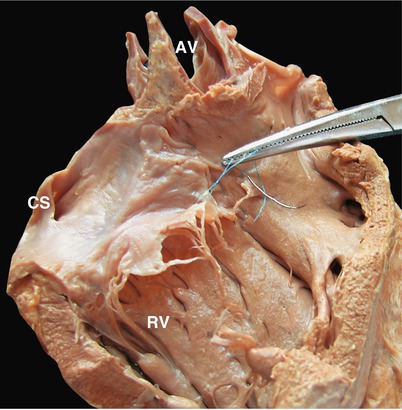
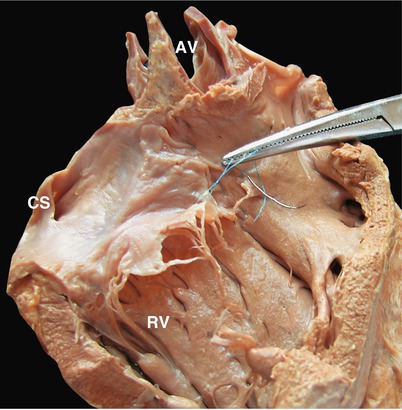
Fig. 4.3
Right ventricle without anterior wall. Viewed from its face side, without the anterior wall, retention of the tricuspid annulus, anterior leaflet of the TV, and the magnitude of the anterior papillary muscle can be seen. In front of the TV, the conical papillary muscle is connected with the supraventricular crest; between the right ventricular outflow tract and the aorta is the reflection of the infundibulum. AO aortic root, CS coronary sinus, RA right atrium, RV right ventricle
Right ventricular incisions are limited by the branches of the conus arteriosus from the right coronary artery, injury to which should be avoided. An infundibular incision is useful to display the pulmonary valve and the subvalvular structure, but not the membranous portion.
A larger right ventricular incision or violent pull will damage the right ventricular muscle, affecting the right ventricular systolic function. In some cases, a massive right ventricular branch from the right coronary artery crosses the right ventricular anterior wall, and a right ventricular incision may injure this giant branch, leading to localized myocardial infarction (Fig. 4.4).
Fig. 4.4
Right ventricle used as the operation incision area. The principle for right ventricular incision is to avoid the important branches of the coronary arteries and the tricuspid anterior papillary muscle. The right bundle branch runs along the moderator band, cutting of which can cause a blockage of the right bundle branch and a decrease in the right ventricular contractility. In figure (b) for the anterior papillary muscle, the dotted box shows the area where a right ventricular incision can be made
4.3 Right Ventricular Cavity Divisions
The right ventricular cavity is divided into three portions (Figs. 4.5, 4.6, and 4.7):
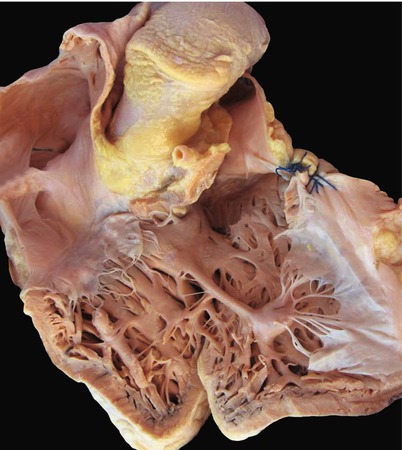
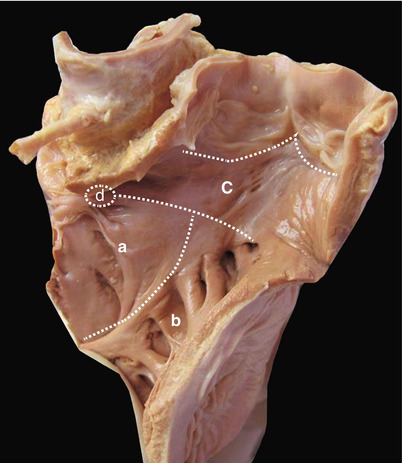
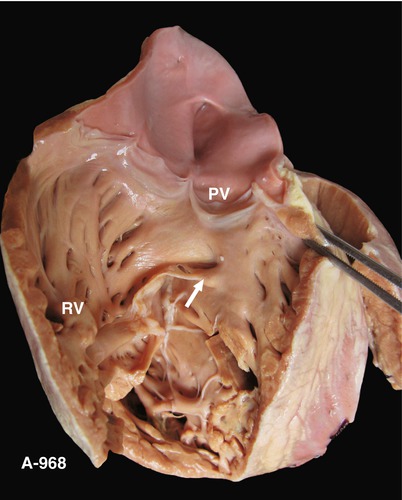
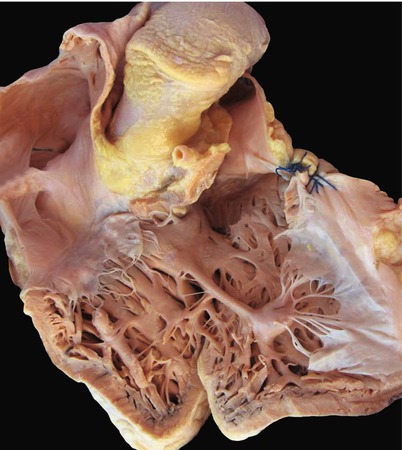
Fig. 4.5
Right ventricular cavity. The right ventricular cavity can be divided into three parts: (1) the right ventricular inflow part (namely, the sinus), which has a smooth inner wall and an upper edge formed by the TV annulus, also including membranous ventricular septal; (2) the apical area of trabecular portion; and (3) the right ventricular infundibulum, also referred to as the outflow portion, the distal end of which is connected to the main pulmonary artery
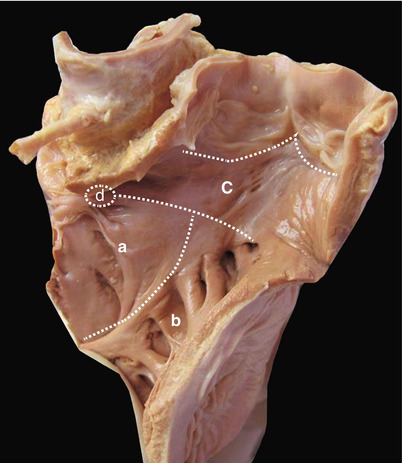
Fig. 4.6
Interventricular septum viewed from the right ventricle. From this view, the interventricular septum can be divided into four portions: (a) the ventricular inflow tract or sinus, which has the smooth inner wall; (b) the trabecular portion, where many bundles are present; (c) the right ventricular outflow tract as the infundibulum, a supraventricular crest connects with the sinus; (d) the membranous septum, which is very small, is in front of the tricuspid septal leaflet, and is positioned below the conical papillary muscle
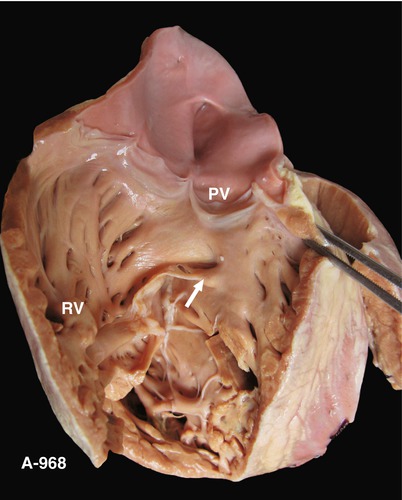
Fig. 4.7
Right ventricular flow tract. The right ventricular flow tract between the pulmonary valve and the TV is seen, along with infundibular muscular tissue under the pulmonary valve; there is no continuous fiber between the pulmonary valve and TV. Arrow cone papillary muscle, PV pulmonary valve
4.3.1 Sinus Portion
The right ventricular sinus portion is the right ventricular inflow tract (Fig. 4.8). It is formed by embryonic, primitive, muscular ventricular septal growth. The inner wall is smooth. The TV apparatus can be seen in this portion.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


