The Respiratory System and Auscultation
ANATOMY AND PHYSIOLOGY
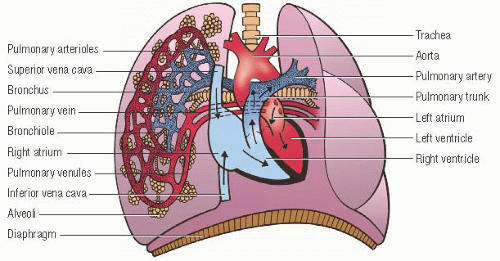
The primary function of the respiratory system is the exchange of oxygen (O2) and carbon dioxide (CO2) between the alveoli and the pulmonary circulation.
During inspiration, air enters the upper airway and travels through the lower airways until it reaches the alveoli. Each alveolus is surrounded by multiple capillaries. During systole, deoxygenated blood returning from the body’s cells is pumped from the right ventricle through the arterial pulmonary circulation to the alveolar capillaries. CO2 diffuses from the capillary blood across the alveolar capillary membrane and enters the alveolar air. Simultaneously, O2 from the inspired atmospheric air in the alveolus crosses the alveolar capillary membrane and enters the pulmonary capillary blood.
During expiration, CO2 is exhaled from the lungs. Oxygenated capillary blood travels to the left side of the heart and is pumped from the ventricle into arterial circulation to the cells of the body, where cellular respiration occurs.
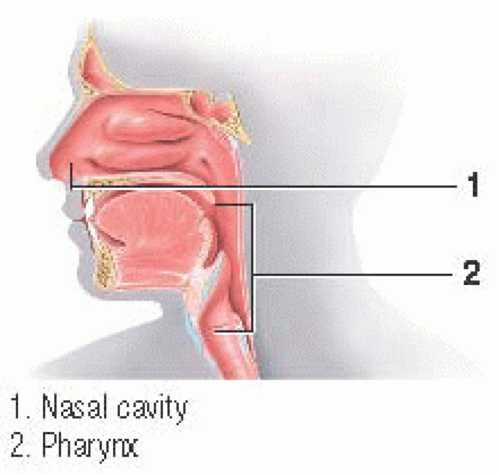
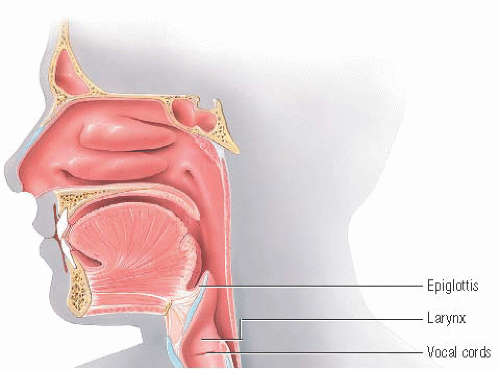
Upper airway
The upper airway consists of the nasal cavities and the pharynx. Air enters the body through the nostrils and passes through the nasal cavities. Vibrissae located in the nostrils filter out foreign
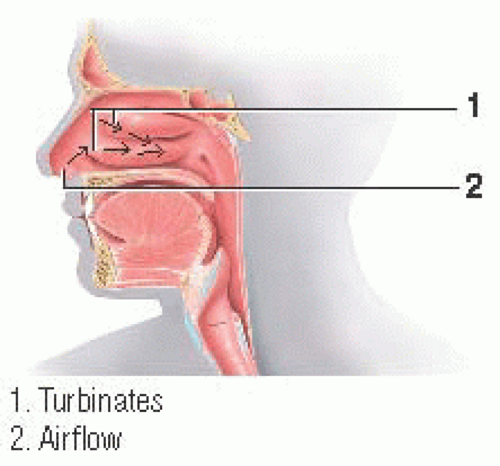
particles. The lateral walls of the nasal cavities curve, forming turbinates (conchae), which increase the mucosal surface area and produce turbulent airflow.
particles. The lateral walls of the nasal cavities curve, forming turbinates (conchae), which increase the mucosal surface area and produce turbulent airflow.
The lining of the nasal cavities contains a dense capillary network and serous glands that warm and humidify the inspired air. Seromucous glands produce a sticky film over the lining that traps particles against it during airflow.
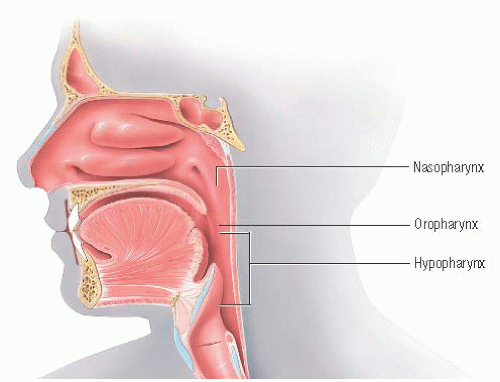
The pharynx is divided into three sections: the nasopharynx, the oropharynx, and the hypopharynx. The nasopharynx begins at the posterior openings of the nasal cavities and extends to the soft palate; the oropharynx, the middle section, is the common passageway for food and air; and the hypopharynx, the lower section, extends from the roof of the tongue to the glottic area.
In children, the larynx and glottis are positioned higher in the neck, creating a greater risk for aspiration.
Lower airway
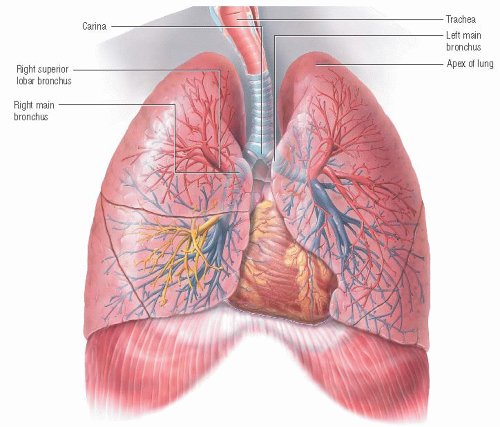
The lower airway is called the tracheobronchial tree. It begins at the level of the cricoid cartilage of the larynx and ends at the distal bronchioles, which open into the alveoli.
The larynx, which contains the epiglottis and vocal cords, has a role in ventilation and phonation and helps protect the lower airway from aspiration.
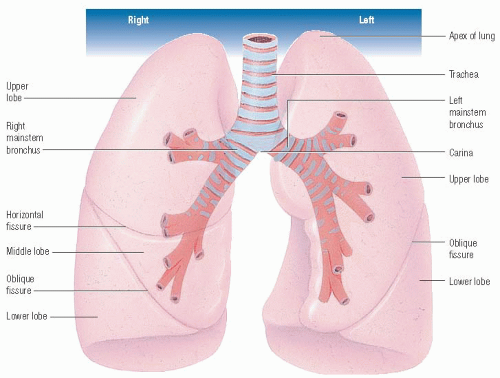
Trachea
The adult trachea is about 1” (2.5 cm) in diameter and 4” (10 cm) long to the bifurcation, which is also called the carina. Anteriorly, the trachea begins just below the larynx and is located within the thoracic cavity, beneath the upper two-thirds of the sternum. Posteriorly, it begins at the level of the sixth cervical or first thoracic vertebra and extends to about the fifth thoracic vertebra.
In children, the trachea is shorter with a more acute angle at the bifurcation of the right bronchus. The smaller diameter of the trachea results in increased airway resistance.
Mainstem bronchus
The trachea divides into a right and left mainstem bronchus. The left mainstem bronchus leaves the trachea at a sharper angle than the right mainstem bronchus and passes under the aortic arch before entering the lung. The mainstem bronchi enter the lungs at the hila, where the lung tissue attaches to the mediastinum. The bronchi course downward and immediately divide into lobar bronchi, which subdivide into segmental bronchi.
The airways continue to systematically branch, narrow, shorten, and increase in number toward the lung periphery. They divide about 25 times before ultimately opening into the terminal, or respiratory, bronchioles.
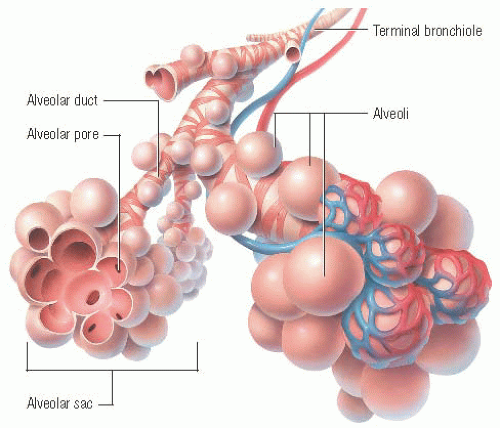
Terminal bronchioles
The terminal bronchioles, which have a few alveoli budding from their walls, branch into alveolar ducts that are completely lined with alveoli. Known as the respiratory zone, this area is where gas exchange occurs. These airways and their alveoli form the respiratory lobules of the lungs. The terminal bronchioles account for the last six or seven airway divisions. The distance from the terminal bronchiole to the most distal alveolus is only about 5 mm; however, most of the lung surface area available for gas exchange is contained in these spaces.
Conducting airways
The airways between the nose and the terminal bronchioles— called the conducting airways—lead inspired gas to the gas exchange regions of the lungs. About 150 cc of inspired air remains in the conducting airways during each breath. These airways, called anatomic dead space, aren’t involved in gas exchange.
The large airways below the glottis contain cartilage, smooth muscle, elastic fibers, connective tissue, and mucous glands. Anteriorly, the trachea and mainstem bronchi are composed of 20 rings of U-shaped cartilage. The cartilage that
opens posteriorly is connected by a band of smooth muscle and fibroelastic tissue. About 30% of the wall thickness in the mainstem and lobar bronchi is cartilage. This cartilage becomes irregular and platelike and eventually disappears in the smaller airways, which consist solely of smooth muscle and elastic fibers.
opens posteriorly is connected by a band of smooth muscle and fibroelastic tissue. About 30% of the wall thickness in the mainstem and lobar bronchi is cartilage. This cartilage becomes irregular and platelike and eventually disappears in the smaller airways, which consist solely of smooth muscle and elastic fibers.
The mucous and bronchial glands located in the bronchial walls secrete a serous mucus blanket onto the inside airway walls. This secreted mucus forms a thin, sticky layer that lies atop ciliated columnar epithelial cells, which line nearly all of the respiratory tract between the larynx and the terminal bronchioles. The mucus layer traps foreign particles in the inspired air before they can enter the lungs. Cilia move in a wavelike motion, propelling the sticky mucus layer toward the pharynx where it can be coughed out or swallowed. Together, the mucus layer and cilia protect the lungs, acting as a major defense mechanism against inhaled particles.
Lung lobes
Each lung is divided into lobes. The right lung has three lobes: the upper, middle, and lower. The left lung has only an upper and a lower lobe. The lung’s apex (superior aspect) is located near the clavicle, and its base (inferior aspect) is located near the diaphragm. (See Lung lobes, page 110.)
Alveoli
The terminal bronchioles divide into two to five alveolar ducts, each of which consists of 10 to 16 alveoli. Alveoli contain three cell types. Type I, the largest, is the lining cell and accounts for 95% of the alveolar surface area. The type II cell produces surfactant, a mixture of phospholipids. The macrophage, the third cell type, acts as a phagocytic defense mechanism against infection.
The adult respiratory system contains about 300 million alveoli. In a healthy adult, the surface area of the alveolar-capillary membrane available for O2-CO2 exchange is 70 to 85 m2, about the size of a tennis court.
Adults have about 10 times the number of alveoli as infants, who have alveoli that are larger with less elastic recoil. The number of alveoli reaches that of an adult by age 12.
The alveolar surface is covered by a fluid layer containing surfactant. The surfactant mixes with pulmonary fluids and maintains alveolar stability by lowering the alveolar surface tension. This action protects against atelectasis and hypoxia by preventing the air-filled alveoli from collapsing at low volumes from the weight of capillary blood.
In older adults, elastic recoil in the alveoli decreases and surface area for gas exchange is reduced as alveoli septa are lost.
Lower airway innervation
Two neural pathways, the parasympathetic and sympathetic nervous systems, innervate the tracheobronchial tree. The relative balance of the two neural pathways and their effect on the smooth muscle, which lines the tracheobronchial tree, results in bronchial smooth muscle tone.
The parasympathetic nervous system in the larynx, trachea, and bronchi includes vagal nerve fibers and irritant receptors mediated by the neurotransmitter acetylcholine. Parasympathetic stimulation precipitates bronchoconstriction, coughing, and mucus discharge from the bronchial glands. Irritant receptors within the airways are believed to be responsible for increasing ventilation and precipitating coughing.
Sympathetic innervation of the lower airways usually arises from the thoracic nerves T1 through T5 and is mediated by the
postganglionic hormone transmitter norepinephrine. Sympathetic stimulation of beta2-adrenergic receptors throughout the lower airways facilitates smooth muscle relaxation, resulting in bronchodilation.
postganglionic hormone transmitter norepinephrine. Sympathetic stimulation of beta2-adrenergic receptors throughout the lower airways facilitates smooth muscle relaxation, resulting in bronchodilation.
The secretory mast cells on the surface of the large airways also may be stimulated or affected by drugs, hormones, antigens, and other messenger cells to precipitate or control bronchoconstriction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree