The Left Ventricle and Its Systolic Function
ECHO ASSESSMENT OF THE LEFT VENTRICLE
In many echo departments, assessment of left ventricular (LV) function is the single commonest echo request. One reason for this is that symptoms and signs that can indicate heart failure are common and echo is a noninvasive, straightforward and relatively inexpensive technique for confirming whether LV dysfunction is present. This chapter will cover the assessment of LV dimensions and overall LV systolic function. The assessment of regional systolic function, in the context of coronary artery disease, is discussed in Chapter 16, and left ventricular diastolic function is covered in Chapter 17.
The key challenge in using echo to assess the LV lies in summarizing the size and function of a complex 3D structure using just a handful of parameters. Trying to represent the LV within a limited number of measurements is fraught with pitfalls, not least when using volumetric measures that rely on assumptions about the geometrical shape of the LV, which are not necessarily correct, particularly if the shape of the LV is distorted or abnormalities are limited just to one or two areas of the ventricular wall. The key is to use common sense – if there is a clear discrepancy between your ‘eyeball’ assessment of the LV and the figures coming out of your calculations, highlight this in your report.
LV dimensions
LV shape
wall thickness
cavity size
LV mass
LV systolic function
global function
regional function (see Chapter 16)
LV diastolic function (see Chapter 17)
LV masses or thrombus (see Chapter 27).
If you haven’t already done so, you may also find it helpful to read the chapters on tissue Doppler imaging (Chapter 10) and myocardial mechanics and speckle tracking (Chapter 11).
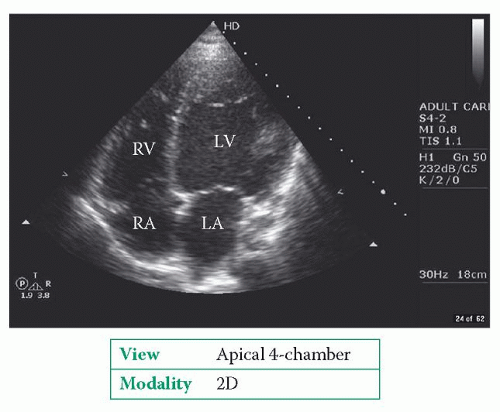
LEFT VENTRICULAR DIMENSIONS
In measuring LV dimensions it is important not to ‘miss the wood for the trees’ – as LV measurements only provide a selective snapshot of the LV in the regions where the measurements are taken, you must ensure that your report also includes a description of any abnormalities that are not reflected in the figures alone. Take the time to ‘eyeball’ the LV as a whole in several views (at least part of the LV is visible in almost every standard view of the heart) and if the overall shape is abnormal, be sure to describe this (Fig. 15.1). A good example of this is the presence of an LV aneurysm, in which case describe its location and identify whether it is a true aneurysm or a pseudoaneurysm (Chapter 16), or the presence of a localised area of hypertrophy in hypertrophic cardiomyopathy.
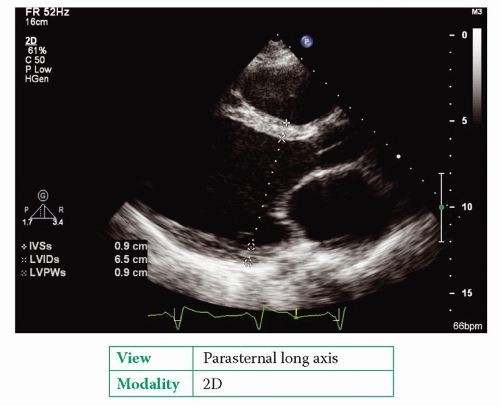
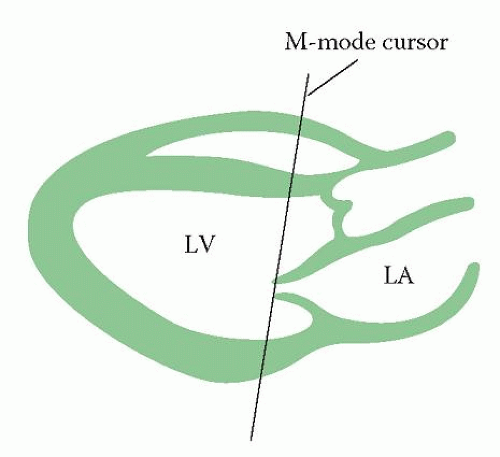
Linear LV measurements
Next, take some measurements of the LV wall and cavity dimensions in both systole and diastole. Linear LV measurements can be taken directly from a 2D echo image (Fig. 15.2), or using M-mode echo if you prefer (Fig. 15.3), in either the parasternal
long axis or parasternal short axis view at the level of the mitral valve leaflet tips. Although M-mode has the advantage of high temporal resolution, making it easier to visualize motion of the endocardium, it is nonetheless easier to ensure correct alignment of your measurements (i.e. at 90° to the long axis of the LV cavity) if you take them directly from the 2D image. Whatever technique you prefer, be sure to identify end-diastole and end-systole (see box) and the endocardial/epicardial borders correctly.
long axis or parasternal short axis view at the level of the mitral valve leaflet tips. Although M-mode has the advantage of high temporal resolution, making it easier to visualize motion of the endocardium, it is nonetheless easier to ensure correct alignment of your measurements (i.e. at 90° to the long axis of the LV cavity) if you take them directly from the 2D image. Whatever technique you prefer, be sure to identify end-diastole and end-systole (see box) and the endocardial/epicardial borders correctly.
END-DIASTOLE AND END-SYSTOLE
End-diastolic measurements are often taken at the onset of the QRS complex on the ECG trace. However, the American Society of Echocardiography (ASE) recommends that end-diastole is taken as the frame after mitral valve closure or the frame in the cardiac cycle in which the LV internal dimension is largest.
End-systolic measurements are often taken as the point when the LV internal dimension is at its narrowest, but the ASE also suggests using the frame preceding mitral valve opening as an alternative. The apical 2-chamber view does not show mitral valve opening very well, and so do not base measurements taken in this view on the timing of mitral valve opening.
Starting at the right ventricular (RV) border of the interventricular septum, use the callipers to measure the diastolic LV dimensions:
IVSd (interventricular septal wall dimension – diastole)
Then repeat the process for the systolic LV dimensions:
IVSs (interventricular septal wall dimension – systole)
In the past it has been recommended that such M-mode measurements be taken from leading edge to leading edge, but the improved resolution of contemporary echo machines means that measurements can instead be taken directly from the tissue-blood interface. The echo machine will display the measurements as you make them, and will often also display a number of calculated parameters (e.g. ejection fraction, fractional shortening) based on these measurements (Fig. 15.2).
It is a good idea to make several measurements on different cardiac cycles and obtain an average. It is also possible to adjust the LV internal dimensions for the patient’s body surface area (BSA), measured in square metres. The Mosteller formula is commonly used to calculate BSA:
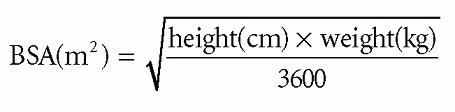
Table 15.1 shows the reference ranges for men and women.
Table 15.1 Reference ranges for men and women | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
COMMON PITFALLS
Pitfalls in the assessment of LV dimensions include:
failure to take measurements at the correct time points (end-systole or end-diastole)
failure to take measurements perpendicular to the long axis of the LV
failure to identify the endocardium correctly – be particularly careful to avoid mistaking chordae tendineae for the endocardium of the LV posterior wall.
Volumetric left ventricular measurements
Volumetric measurements are based upon the principle that LV volumes can be calculated from 2D measurements of the LV as long as certain assumptions about the shape of the LV apply. The more distorted the LV (e.g. as a result of an aneurysm), the less reliable such volumetric measurements become.
Modified Simpson’s rule method
Modified Simpson’s rule method is the best (and most commonly used) way of calculating LV volumes. It is also known as the biplane method of discs, as it works on the principle that the LV cavity can be considered as a stack of elliptical discs of
differing sizes from base to apex. If the volume of each disc is known (from its area and thickness), then the overall LV volume is equal to the volume of all the discs added together.
differing sizes from base to apex. If the volume of each disc is known (from its area and thickness), then the overall LV volume is equal to the volume of all the discs added together.
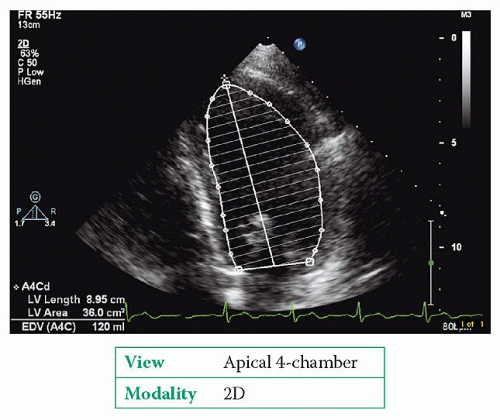
Echo machines automate much of the process and require the operator simply to measure the length of the LV (long axis) and to trace the outline of the LV endocardium in one (or preferably two) planes. To do this:
1. In the apical 4-chamber view obtain the best view you can of the LV, paying particular attention to endocardial border definition and avoidance of foreshortening. The use of an echo contrast agent (Chapter 9) may help delineate the endocardium if the image quality is suboptimal.
2. Freeze a loop and find the end-diastolic image. Now trace the endocardial border from the mitral valve annulus all the way down to the apex and then back up to the annulus on the opposite side. Ignore any papillary muscle that may be visible. The machine will normally join up the start and finish points with a straight line across the mitral valve, to enclose the entire LV cavity within the traced area. The machine will then automatically split the traced area into a stack of discs (usually 20).
3. Measure the length of the LV long axis from the apex to the mid-point of the mitral valve. The machine will now use these measurements to calculate LV enddiastolic volume (LVEDV, Fig. 15.4).
4. Scroll to the end-systolic frame and repeat steps 2 and 3 to obtain the LV endsystolic volume (LVESV).
5. Although a measurement taken in just one plane will give you a value for LVEDV and LVESV, this does make the assumption that each of the discs is circular. Repeating the measurements in the apical 2-chamber view takes better account of the elliptical cross-section of the LV and any regional wall motion abnormalities.
Area-length method
The area-length method can be useful for estimating LV volumes when the endocardium cannot be seen clearly enough to allow accurate tracing. However, it does make major assumptions (and simplifications) about the shape of the LV:
1. In the parasternal short axis view, mid-LV (papillary muscle) level, freeze a loop and find the end-diastolic frame. Perform planimetry by tracing the endocardial border to calculate the cross-sectional area of the LV cavity at this level in cm2. Ignore the presence of the papillary muscles as you trace the endocardium.
2. In the apical 4-chamber view, in the end-diastolic frame, measure the length of the LV long axis from the apex to the mid-point of the mitral valve in cm.
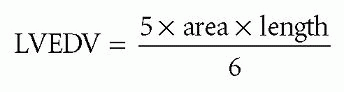
3. The LVEDV, in mL, is given by:
4. Scroll to the end-systolic frame and repeat steps 1 to 3 to obtain the LVESV.
Both LVEDV and LVESD can be adjusted for BSA (‘LV volume index’). Table 15.2 shows the reference ranges for males and females.
Table 15.2 Left ventricle volumes – reference ranges | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|