Chapter 19 The Difficult Abdominal Wall
Acute Presentation
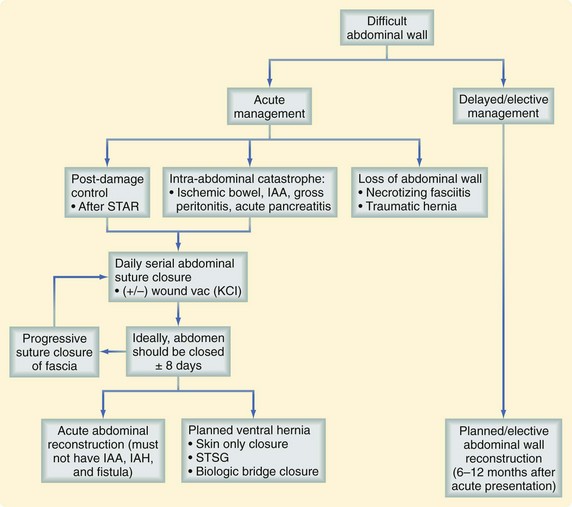
Definitions and Management
Stone and Lucas and colleagues1,2 in the 1980s and Rotondo and Morris3,4 and associates in the 1990s defined the primary goals of damage control surgery in the trauma patient, which included the initial three phases we know today. Fabian and coworkers5 have described the five phases of damage control surgery, from the initial operation to restoration of abdominal wall integrity:
During phase 3, the abdominal fascia is closed more than 65% of the time. All intra-abdominal injuries are repaired, peritonitis controlled, and other disease states corrected. However, there may still be unresolved visceral edema and/or loss of domain with retraction of the abdominal wall. This is the most common scenario giving rise to the difficult abdominal wall. The goal of delayed primary fascial closure is to have the fascia closed within 8 days. Complications increase exponentially after this point, including intra-abdominal abscess and formation of intestinal fistulas, which can increase to 25% to 45%.6 However, the risk of developing intra-abdominal hypertension or abdominal compartment syndrome, ongoing inflammatory response syndrome, lack of source control, and/or intra-abdominal abscess or intestinal fistula may be reason enough to delay primary closure of the abdominal fascia (Box 19-1).
Intra-Abdominal Hypertension or Abdominal Compartment Syndrome Complicating the Difficult Abdominal Wall
Once reexploration and staged abdominal reconstruction have been completed, the next goal is to close the abdomen with the least amount of physiologic stress. Intra-abdominal hypertension is known to cause ischemia to the viscera and abdominal wall, which can progress to abdominal compartment syndrome with organ dysfunction. In 2004, the World Congress of Abdominal Compartment Syndrome met to develop consensus definitions for intra-abdominal hypertension and abdominal compartment syndrome.7,8 These consensus definitions are used to define intra-abdominal hypertension and primary, secondary, and recurrent abdominal compartment syndrome. The World Congress of Abdominal Compartment Syndrome definitions have helped further define the disease processes of intra-abdominal hypertension and abdominal compartment syndrome (Boxes 19-2 and 19-3). Abdominal compartment syndrome is not necessarily an end stage process but a continuum of disease, which might be amenable to medical management at an earlier stage. Grade III intra-abdominal hypertension (intra-abdominal pressure >20 mm Hg) should be further monitored with intravesicular pressure monitoring. Medical therapies should be instituted at this point—supine positioning, judicious crystalloid resuscitation, and drainage of intra-abdominal fluid collections.9 If these fail to improve intra-abdominal hypertension or organ dysfunction develops, serious consideration must be given to decompressive laparotomy. Other therapies to decrease intra-abdominal hypertension may include neuromuscular blockade, increased sedation, diuresis, evacuation of intra-luminal contents, and hemodialysis or hemofiltration.
Box 19-2 World Congress Abdominal Compartment Syndrome Definitions
Intra-Abdominal Hypertension and Abdominal Compartment Syndrome
Normal intra-abdominal pressure is ≈5-7 mm Hg in critically ill adults.
Intra-abdominal hypertension is graded as follows (in mm Hg):
Box 19-3 Types of Abdominal Compartment Syndrome
Abdominal decompression lowers intra-abdominal hypertension and results in improvement in lung dynamic compliance.10 Bladder pressures higher than 25 mm Hg have been suggested to indicate abdominal compartment syndrome.11 Using the definition of abdominal compartment syndrome—the development of significant respiratory compromise, including elevated inspiratory pressure (≈35 cm H2O), renal dysfunction (urine <30 mL/hr), hemodynamic instability requiring catecholamines, and a rigid or tense abdomen, it has been found that in these patients, emergency abdominal decompression results in a significant increase in the cardiac index, tidal volume, and urine output, with a resultant decrease in bladder pressure, heart rate, central venous pressure, pulmonary artery occlusion pressure, peak airway pressure, partial pressure of arterial carbon dioxide, and lactate level. Abdominal decompression may also be of benefit in the setting of increased intracranial pressure.
Secondary abdominal compartment syndrome may occur after exsanguination from an extremity injury and/or when massive volume resuscitation is required. Recurrent abdominal compartment syndrome occurs after damage control in a patient with an open abdomen with ongoing hemorrhage or massive volume resuscitation. In all scenarios, intra-abdominal pressure should be monitored.12,13
Abdominal Catastrophe Complicating the Difficult Abdominal Wall
Tissue loss of the abdominal wall posses a uniquely difficult problem. Blast, shear, and penetrating traumatic injuries and necrotizing skin and soft tissue infections can all result in significant tissue loss. Loss of abdominal wall tissue will require creative temporary abdominal closure, with the goal of maintaining integrity of the bowel. In these clinical scenarios, a definitive repair of the abdominal wall defect may require the use of autologous tissue or biologic or synthetic mesh. In severe cases, acute primary repair of the ventral hernia is not recommended because of the high incidence of gastrointestinal contamination, resolving source control of infection, and continued risk of wound infection. In these cases, synthetic mesh is contraindicated because of the high risk of mesh infection.14
Other Conditions Complicating the Difficult Abdominal Wall
After the abdomen has been opened, adhesions develop and the viscera will become cocooned. This makes reexploration of the bowel for fistula repair or bowel obstructions almost impossible without causing further injury. The development of bowel fistula will commonly occur at the site of an anastomosis, but may be in exposed small bowel not previously injured.6,15
After any traumatic or emergency laparotomy in which bleeding and gastrointestinal injury occurred, the risk of an intra-abdominal abscess can be as high as 25% to 35%.6 Most intra-abdominal abscesses can be percutaneously drained, but may still require open drainage. In the setting of intra-abdominal abscess, enteroatmospheric fistula, tissue loss, loss of abdominal domain, and massive visceral edema, the safest course in an open abdomen is to proceed with a planned ventral hernia.
Temporary Abdominal Closure
Techniques
The development of the open abdomen technique has posed a new problem—how to close the abdomen temporarily in a way that is easy to apply, tension-free, atraumatic, and inexpensive, and allows for a high rate of delayed primary fascial closure. The options for temporary abdominal closure can be broadly classified as dynamic (securing a device to the fascial edges for serial approximation to achieve delayed primary fascial closure) or tension-free (atraumatic abdominal visceral coverage). Current and historical techniques are presented in Table 19-1. The most widely used delayed primary fascial closure techniques now used in the United States are the artificial burr, vacuum pack, and commercially available vacuum pack device.
Table 19-1 Current and Historical* Techniques for Temporary Abdominal Closure
| TECHNIQUE | DESCRIPTION | MECHANISM |
|---|---|---|
| Vacuum-assisted closure (VAC) | A perforated plastic sheet covers the viscera and a sponge is placed between the fascial edges. The wound is covered by an airtight seal, which is pierced by a suction drain connected to a suction pump and fluid collection system. | The (active and adjustable) negative pressure supplied by the pump keeps constant tension on the fascial edges while it collects excess abdominal fluid and helps resolve edema. |
| Vacuum pack | A perforated plastic sheet covers the viscera, damp surgical towels are placed in the wound, and a surgical drain is placed on the towels. An airtight seal covers the wound and negative pressure is applied through the drain. | The negative pressure keeps constant tension on the fascial edges and excess fluid is collected. |
| Artificial burr (Wittmann patch) | Two opposite Velcro sheets (hooks and loops, one on each side) are sutured to the fascial edges. The Velcro sheets connect in the middle. | This technique allows for easy access and stepwise reapproximation of the fascial edges. |
| Dynamic retention sutures | The viscera are covered with a sheet (e.g., ISODrape, Microtek [Microban], Huntersville, NC). Horizontal sutures are placed through a large-diameter catheter and through the entire abdominal wall on both sides. | The sutures keep tension on the fascia and may be tightened to allow staged reapproximation of the fascial edges. This may be combined with a vacuum system. |
| Plastic silo (Bogota bag) | A sterile x-ray film cassette bag or sterile 3-liter urology irrigation bag is sutured between the fascial edges or the skin and opened in the middle. | This is an easy technique that allows for easy access. The bag may be reduced in size to approximate the fascial edges. |
| Mesh, sheet | An absorbable or nonabsorbable mesh or sheet is sutured between the fascial edges. Examples are Dexon, Marlex, or Vicryl mesh. Examples of sheets are Silastic or silicone sheets. | The mesh or sheet may be reduced in size to allow for reapproximation. Nonresorbable meshes may be removed or left in place at the end of the open abdominal period. |
| Loose packing* | The fascial defect is covered by standard wound dressing only. | This technique is simple but does not prevent fascial retraction. |
| Skin approximation | The skin is closed over the fascial defect with towel clips or a running suture. | Skin provides a natural cover for the viscera, but the towel clips obstruct radiologic imaging and do not prevent fascial retraction. |
| Zipper* | A mesh or sheet with a sterilized zipper is sutured between the fascial edges. | This technique is comparable to the mesh/sheet and allows for easy access. |
* Denotes a historical technique.
The artificial burr consists of two sheets of hook and burr material, similar to Velcro, that is sewn to the fascial edges after a plastic drape is placed over the viscera. The hook and burr is then overlapped with limited tension to provide a secure temporary abdominal closure. Gauze is used to pack the subcutaneous tissue.16 Pulling the Velcro-like material apart easily allows reexploration of the abdomen. At the completion of the subsequent operations, the patch can be tightened to keep fascial tension. Repeated tightening allows for a sequential approximation of the fascia until it can be closed without undue tension. In 2009, Van Hensbroek and colleagues17 have suggested that the artificial burr, along with dynamic retention sutures paired with a commercially available vacuum pack device, have the highest success in fascial closure rates.
In 1995, Brock and associates18 first described the vacuum pack, which is a three-layer temporary abdominal closure. A fenestrated polyvinyl sheet is draped over the exposed viscera and tucked under the fascial edges. A surgical towel is placed under the fascia, followed by two silicone drains, which are placed on top of the towel. An adhesive, iodophor-impregnated polyester drape is placed over the skin laterally to the anterior axillary lines to seal the wound. The surgical drains are connected to a wall suction, creating a negative-pressure dressing. The vacuum pack–negative-pressure temporary abdominal closure has gained wide acceptance because it can be applied quickly, is inexpensive and atraumatic, and allows for control of abdominal fluids. It is cost-effective. approximately $50/application.17 In most of this trauma population, delayed primary fascial closure was possible at the second laparotomy. Although delayed primary fascial closure is less common in the emergent surgery population, combined fascial closure rates as high as 68% have been demonstrated.19 Fistula and leak rates are no different than with other types of temporary abdominal closure (TAC), with reported fistula rates of 3% to 5%.19,20
A commercial version of the vacuum pack is available. Results have been similar to primary fascial closure and complication rates comparable to the vacuum pack. A modification of the technique, incorporating dynamic serial fascial closure in conjunction with a commercial vacuum pack, has demonstrated 90% delayed primary fascial closure rates. This technique extends beyond the 8-day benchmark, with low complication rates in some series.19,21 A recent review has suggested that the vacuum pack and artificial burr are associated with the highest closure rates as well as the lowest mortality rates.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree